Tuesday Poster Session
Category: GI Bleeding
P3502 - A Tale of Two Tics: A Rare Case of Acute Consecutive Small Bowel and Colonic Diverticular Bleeding
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Heather Gosnell, DO
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Heather Gosnell, DO, Brian Black, MD, Shreya Narayanan, MD
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: For patients with GI bleeds (GIB), evaluation often includes timely EGD, followed by colonoscopy and video capsule endoscopy (VCE) if the bleeding source is not identified. We present a case of acute consecutive small bowel (SB) and colonic diverticular bleeding, underscoring the need for a multimodal approach to care.
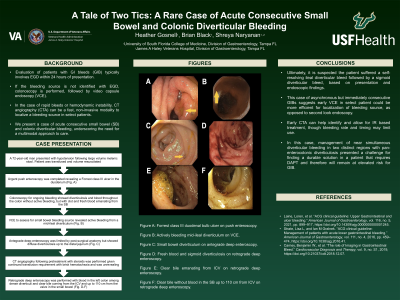
Case Description/Methods: A 72-year-old man with complex abdominal surgical history following gunshot wound and on dual anti-platelet therapy (DAPT) for dialysis graft failure presented with melena. On initial evaluation, he was hemodynamically stable, but then decompensated with hypotension and maroon stools. DAPT was held, he was resuscitated, and emergent push enteroscopy revealed a Forrest class III duodenal bulb ulcer (fig. 1a). For ongoing bleeding, colonoscopy was done and showed pandiverticulosis and blood throughout the colon without active bleeding, but with clot and fresh blood emanating from the SB. VCE completed to localize suspected SB source showed active bleeding from a mid-ileal diverticulum (fig. 1b). Subsequent antegrade deep enteroscopy, limited by post-surgical anatomy, showed SB pandiverticulosis (fig. 1c) without active bleeding up to the distal jejunum. Continued transfusion dependence with brisk hematochezia prompted CT angiography, which was delayed by contrast allergy requiring pretreatment with steroids and was ultimately unrevealing. Retrograde deep enteroscopy was then performed. Fresh blood was seen in the left colon among dense diverticuli (fig. 1d), with minimal old blood in the right colon and clear bile in the SB examined up to 110 cm from the ileocecal valve (fig. 1e, 1f). This suggested a separate, left colon diverticular bleed, though no active GIB was identified. Ultimately, it is suspected the patient suffered a self-resolving ileal diverticular bleed followed by a sigmoid diverticular bleed, based on presentation and endoscopic findings.
Discussion: This case of asynchronous but immediately consecutive SB and colonic diverticular GIB suggests early VCE as opposed to second look endoscopy in select patients would be more efficient for localization of bleeding source. Early CTA can help identify and allow for IR based treatment, though bleeding rate and timing may limit use. In this case, management of near simultaneous diverticular bleeding in two distinct regions with pan-enterocolonic diverticulosis presented a challenge for finding a durable solution in a patient that requires DAPT and therefore will remain at elevated risk for GIB.

Disclosures:
Heather Gosnell, DO, Brian Black, MD, Shreya Narayanan, MD. P3502 - A Tale of Two Tics: A Rare Case of Acute Consecutive Small Bowel and Colonic Diverticular Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University of South Florida Morsani College of Medicine, Tampa, FL
Introduction: For patients with GI bleeds (GIB), evaluation often includes timely EGD, followed by colonoscopy and video capsule endoscopy (VCE) if the bleeding source is not identified. We present a case of acute consecutive small bowel (SB) and colonic diverticular bleeding, underscoring the need for a multimodal approach to care.
Case Description/Methods: A 72-year-old man with complex abdominal surgical history following gunshot wound and on dual anti-platelet therapy (DAPT) for dialysis graft failure presented with melena. On initial evaluation, he was hemodynamically stable, but then decompensated with hypotension and maroon stools. DAPT was held, he was resuscitated, and emergent push enteroscopy revealed a Forrest class III duodenal bulb ulcer (fig. 1a). For ongoing bleeding, colonoscopy was done and showed pandiverticulosis and blood throughout the colon without active bleeding, but with clot and fresh blood emanating from the SB. VCE completed to localize suspected SB source showed active bleeding from a mid-ileal diverticulum (fig. 1b). Subsequent antegrade deep enteroscopy, limited by post-surgical anatomy, showed SB pandiverticulosis (fig. 1c) without active bleeding up to the distal jejunum. Continued transfusion dependence with brisk hematochezia prompted CT angiography, which was delayed by contrast allergy requiring pretreatment with steroids and was ultimately unrevealing. Retrograde deep enteroscopy was then performed. Fresh blood was seen in the left colon among dense diverticuli (fig. 1d), with minimal old blood in the right colon and clear bile in the SB examined up to 110 cm from the ileocecal valve (fig. 1e, 1f). This suggested a separate, left colon diverticular bleed, though no active GIB was identified. Ultimately, it is suspected the patient suffered a self-resolving ileal diverticular bleed followed by a sigmoid diverticular bleed, based on presentation and endoscopic findings.
Discussion: This case of asynchronous but immediately consecutive SB and colonic diverticular GIB suggests early VCE as opposed to second look endoscopy in select patients would be more efficient for localization of bleeding source. Early CTA can help identify and allow for IR based treatment, though bleeding rate and timing may limit use. In this case, management of near simultaneous diverticular bleeding in two distinct regions with pan-enterocolonic diverticulosis presented a challenge for finding a durable solution in a patient that requires DAPT and therefore will remain at elevated risk for GIB.

Figure: 1A) Forrest Class III ulcer in duodenal bulb found on push enteroscopy, hospital day 1.
1B) Actively bleeding diverticulum in mid ileum on VCE, hospital day 2.
1C) Small bowel diverticulum on antegrade single balloon enteroscopy, hospital day 3.
1D) Ileum with non-bloody contents on retrograde single balloon enteroscopy, hospital day 6.
1E) Non-bloody bile emanating from ICV on retrograde single balloon enteroscopy, hospital day 6.
1F) Fresh blood without active bleeding in the sigmoid colon on retrograde single balloon enteroscopy, hospital day 6.
1B) Actively bleeding diverticulum in mid ileum on VCE, hospital day 2.
1C) Small bowel diverticulum on antegrade single balloon enteroscopy, hospital day 3.
1D) Ileum with non-bloody contents on retrograde single balloon enteroscopy, hospital day 6.
1E) Non-bloody bile emanating from ICV on retrograde single balloon enteroscopy, hospital day 6.
1F) Fresh blood without active bleeding in the sigmoid colon on retrograde single balloon enteroscopy, hospital day 6.
Disclosures:
Heather Gosnell indicated no relevant financial relationships.
Brian Black indicated no relevant financial relationships.
Shreya Narayanan indicated no relevant financial relationships.
Heather Gosnell, DO, Brian Black, MD, Shreya Narayanan, MD. P3502 - A Tale of Two Tics: A Rare Case of Acute Consecutive Small Bowel and Colonic Diverticular Bleeding, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
