Tuesday Poster Session
Category: GI Bleeding
P3505 - Isolated Duodenal Variceal Hemorrhage Related to a History of Sleeve Gastrectomy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- VM
Varun Moktan, MD
Prisma Health-Upstate
Greenville, SC
Presenting Author(s)
Award: Presidential Poster Award
Dieu Thao Nguyen1, Coral Holt, BS2, Varun Moktan, MD2, Adrian Pona, MD3, Sean Fitzgerald, DO3, Joseph Beets, MD3, Chauncy Handran, MD4
1University of South Carolina, Greenville, SC; 2Prisma Health-Upstate, Greenville, SC; 3Prisma Health, Greenville, SC; 4Prisma, Greenville, SC
Introduction: Varices are a common sequela of portal hypertension (HTN) with the most common locations in the esophagus and cardio-fundus. Ectopic varices outside of these locations represent 2 to 5% of all variceal hemorrhages. Therefore, patients with a surgical history altering the esophagus or cardio-fundus may have an increased risk of developing ectopic varices. This case reports a patient with cirrhosis and a history of sleeve gastrectomy presenting with hemorrhagic shock secondary to isolated duodenal varices.
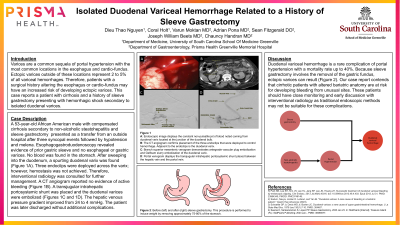
Case Description/Methods: A 53-year-old African American male with compensated cirrhosis secondary to non-alcoholic steatohepatitis and sleeve gastrectomy presented as a transfer from an outside hospital after three syncopal events followed by hypotension and melena. EGD revealed evidence of prior gastric sleeve and no esophageal or gastric varices. No blood was found in the stomach. After sweeping into the duodenum, a spurting duodenal varix (Figure A) was found. Three endoclips were deployed across the varix; however, hemostasis was not achieved. Therefore, interventional radiology was consulted for further management. A CT angiogram (Figure B) reported no evidence of active bleeding; however, a transjugular intrahepatic portosystemic shunt was placed and the duodenal varices were embolized (Figures C and D). The hepatic venous pressure gradient improved from 24 to 4 mmHg. The patient was later discharged without additional complications.
Discussion: Duodenal variceal hemorrhage is a rare complication of portal HTN with a mortality rate up to 40%. Because sleeve gastrectomy involves the removal of the gastric fundus, ectopic varices can result. Our case report contends that cirrhotic patients with altered bariatric anatomy are at risk for developing bleeding from unusual sites. These patients should have close monitoring and early discussion with interventional radiology as traditional endoscopic methods may not be suitable for these complications.

Disclosures:
Dieu Thao Nguyen1, Coral Holt, BS2, Varun Moktan, MD2, Adrian Pona, MD3, Sean Fitzgerald, DO3, Joseph Beets, MD3, Chauncy Handran, MD4. P3505 - Isolated Duodenal Variceal Hemorrhage Related to a History of Sleeve Gastrectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Dieu Thao Nguyen1, Coral Holt, BS2, Varun Moktan, MD2, Adrian Pona, MD3, Sean Fitzgerald, DO3, Joseph Beets, MD3, Chauncy Handran, MD4
1University of South Carolina, Greenville, SC; 2Prisma Health-Upstate, Greenville, SC; 3Prisma Health, Greenville, SC; 4Prisma, Greenville, SC
Introduction: Varices are a common sequela of portal hypertension (HTN) with the most common locations in the esophagus and cardio-fundus. Ectopic varices outside of these locations represent 2 to 5% of all variceal hemorrhages. Therefore, patients with a surgical history altering the esophagus or cardio-fundus may have an increased risk of developing ectopic varices. This case reports a patient with cirrhosis and a history of sleeve gastrectomy presenting with hemorrhagic shock secondary to isolated duodenal varices.
Case Description/Methods: A 53-year-old African American male with compensated cirrhosis secondary to non-alcoholic steatohepatitis and sleeve gastrectomy presented as a transfer from an outside hospital after three syncopal events followed by hypotension and melena. EGD revealed evidence of prior gastric sleeve and no esophageal or gastric varices. No blood was found in the stomach. After sweeping into the duodenum, a spurting duodenal varix (Figure A) was found. Three endoclips were deployed across the varix; however, hemostasis was not achieved. Therefore, interventional radiology was consulted for further management. A CT angiogram (Figure B) reported no evidence of active bleeding; however, a transjugular intrahepatic portosystemic shunt was placed and the duodenal varices were embolized (Figures C and D). The hepatic venous pressure gradient improved from 24 to 4 mmHg. The patient was later discharged without additional complications.
Discussion: Duodenal variceal hemorrhage is a rare complication of portal HTN with a mortality rate up to 40%. Because sleeve gastrectomy involves the removal of the gastric fundus, ectopic varices can result. Our case report contends that cirrhotic patients with altered bariatric anatomy are at risk for developing bleeding from unusual sites. These patients should have close monitoring and early discussion with interventional radiology as traditional endoscopic methods may not be suitable for these complications.

Figure: Figure A: Endoscopic image displays the constant non-pulsatile jet of blood noted coming from duodenal varix located at the junction of the duodenal bulb.
Figure B: The CT angiogram confirms placement of the three endoclips that were deployed to control hemorrhage. Adjacent to the endoclips is the duodenal varix.
Figure C: Branch superior mesenteric venogram demonstrates antegrade vascular plug embolization and Gelfoam slurry embolization of the duodenal varix.
Figure D: Portal venogram displays the transjugular intrahepatic portosystemic shunt placed between the hepatic vein and the portal vein.
Figure B: The CT angiogram confirms placement of the three endoclips that were deployed to control hemorrhage. Adjacent to the endoclips is the duodenal varix.
Figure C: Branch superior mesenteric venogram demonstrates antegrade vascular plug embolization and Gelfoam slurry embolization of the duodenal varix.
Figure D: Portal venogram displays the transjugular intrahepatic portosystemic shunt placed between the hepatic vein and the portal vein.
Disclosures:
Dieu Thao Nguyen indicated no relevant financial relationships.
Coral Holt indicated no relevant financial relationships.
Varun Moktan indicated no relevant financial relationships.
Adrian Pona indicated no relevant financial relationships.
Sean Fitzgerald indicated no relevant financial relationships.
Joseph Beets indicated no relevant financial relationships.
Chauncy Handran indicated no relevant financial relationships.
Dieu Thao Nguyen1, Coral Holt, BS2, Varun Moktan, MD2, Adrian Pona, MD3, Sean Fitzgerald, DO3, Joseph Beets, MD3, Chauncy Handran, MD4. P3505 - Isolated Duodenal Variceal Hemorrhage Related to a History of Sleeve Gastrectomy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

