Tuesday Poster Session
Category: GI Bleeding
P3517 - Development of Diffuse Upper Gastrointestinal Tract Submucosal Petechiae and Haemorrhage in a Patient With Newly Diagnosed Primary Immune Thrombocytopenic Purpura
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kayla Dadgar, MD
McMaster University
Hamilton, ON, Canada
Presenting Author(s)
Yuxuan Jiang, BSc1, Kayla Dadgar, MD2, Christopher Stallwood, MD2, Helena Lau, MD, FRCPC3
1Michael G. DeGroote School of Medicine, McMaster University, Hamilton, ON, Canada; 2McMaster University, Hamilton, ON, Canada; 3Oakville Trafalgar Memorial Hospital, Halton Healthcare, Oakville, ON, Canada
Introduction: Symptom-producing GI bleed due to primary immune thrombocytopenic purpura (ITP) remains highly uncommon, and patients' hypocoagulability pose challenge for endoscopic interventions.
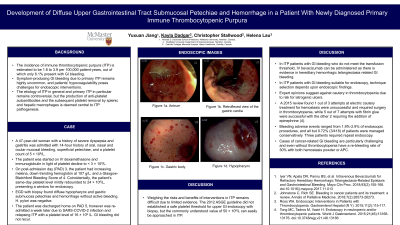
Case Description/Methods: A 47-year-old woman with a distant history of severe dyspepsia and gastritis was admitted with 14-hour history of oral, nasal and ocular mucosal bleeding, superficial petechiae, and a platelet count of 5 × 109/L. The patient was started on IV examethasone and immunoglobulin in light of platelet decline to < 3 × 109/L. On post-admission day (PAD) 3, the patient had increasing melena, down-trending Hgb at 107 g/L, and a Glasgow-Blatchford Bleeding Score of 4. Coincidentally, the patient’s same-day platelet level mildly rebounded to 24 × 109/L, presenting a window for endoscopy. EGD with biopsy found diffuse hypopharynx and gastric submucosa petechiae and hemorrhage without active bleeding. H. pylori was negative. The patient was discharged home on PAD 5, however was re-admitted a week later due to SARS-COVID-2 infection and relapsing ITP with a platelet level of 16 × 109 /L. No GI bleed recurred.
Discussion: Weighing the risks and benefits of interventions in ITP remain difficult due to limited evidence. The 2012 ASGE guideline has not established a safe platelet threshold for upper GI endoscopy with biopsy, but the commonly understood value of 0.05 × 109/L can easily be approached in ITP.
In ITP patients with GI bleed unsuitable for endoscopic and did not meet transfusion threshold, IV bevacizumab could be attempted for its evidence in hereditary haemorrhagic telangiectasia GI bleed.
In ITP patients with GI bleed suitable for endoscopy, technique selection depends upon endoscopic findings. Although a Canadian RCT found neither argon plasma coagulation (APC) nor hamoclipping to be superior for high-risk ulcers, the former were more likely to fail in ITP. MDACC expert opinions suggested against cautery in thrombocytopenia due to risk for iatrogenic ulcers. A 2015 systematic review found 1 out of 3 attempted electric cautery for haemostasis was unsuccessful and required surgery in thrombocytopenia, while five out of seven attempts with fibrin glue were successful. A survey of patients with advanced cancer requiring GI haemostasis revealed a re-bleeding rate of 30% with both haemostasis powder or APC. In cases of refractory bleeding, radiofrequency ablation could be attempted given its recent validation as a safe and effective treatment for refractory gastric antral vascular ectasia (GAVE).

Disclosures:
Yuxuan Jiang, BSc1, Kayla Dadgar, MD2, Christopher Stallwood, MD2, Helena Lau, MD, FRCPC3. P3517 - Development of Diffuse Upper Gastrointestinal Tract Submucosal Petechiae and Haemorrhage in a Patient With Newly Diagnosed Primary Immune Thrombocytopenic Purpura, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Michael G. DeGroote School of Medicine, McMaster University, Hamilton, ON, Canada; 2McMaster University, Hamilton, ON, Canada; 3Oakville Trafalgar Memorial Hospital, Halton Healthcare, Oakville, ON, Canada
Introduction: Symptom-producing GI bleed due to primary immune thrombocytopenic purpura (ITP) remains highly uncommon, and patients' hypocoagulability pose challenge for endoscopic interventions.
Case Description/Methods: A 47-year-old woman with a distant history of severe dyspepsia and gastritis was admitted with 14-hour history of oral, nasal and ocular mucosal bleeding, superficial petechiae, and a platelet count of 5 × 109/L. The patient was started on IV examethasone and immunoglobulin in light of platelet decline to < 3 × 109/L. On post-admission day (PAD) 3, the patient had increasing melena, down-trending Hgb at 107 g/L, and a Glasgow-Blatchford Bleeding Score of 4. Coincidentally, the patient’s same-day platelet level mildly rebounded to 24 × 109/L, presenting a window for endoscopy. EGD with biopsy found diffuse hypopharynx and gastric submucosa petechiae and hemorrhage without active bleeding. H. pylori was negative. The patient was discharged home on PAD 5, however was re-admitted a week later due to SARS-COVID-2 infection and relapsing ITP with a platelet level of 16 × 109 /L. No GI bleed recurred.
Discussion: Weighing the risks and benefits of interventions in ITP remain difficult due to limited evidence. The 2012 ASGE guideline has not established a safe platelet threshold for upper GI endoscopy with biopsy, but the commonly understood value of 0.05 × 109/L can easily be approached in ITP.
In ITP patients with GI bleed unsuitable for endoscopic and did not meet transfusion threshold, IV bevacizumab could be attempted for its evidence in hereditary haemorrhagic telangiectasia GI bleed.
In ITP patients with GI bleed suitable for endoscopy, technique selection depends upon endoscopic findings. Although a Canadian RCT found neither argon plasma coagulation (APC) nor hamoclipping to be superior for high-risk ulcers, the former were more likely to fail in ITP. MDACC expert opinions suggested against cautery in thrombocytopenia due to risk for iatrogenic ulcers. A 2015 systematic review found 1 out of 3 attempted electric cautery for haemostasis was unsuccessful and required surgery in thrombocytopenia, while five out of seven attempts with fibrin glue were successful. A survey of patients with advanced cancer requiring GI haemostasis revealed a re-bleeding rate of 30% with both haemostasis powder or APC. In cases of refractory bleeding, radiofrequency ablation could be attempted given its recent validation as a safe and effective treatment for refractory gastric antral vascular ectasia (GAVE).

Figure: Figure 1. Diffuse sub-mucosal haemorrhage and petechiae of the gastric body as seen during esophagogastroduodenoscopy (EGD).
Disclosures:
Yuxuan Jiang indicated no relevant financial relationships.
Kayla Dadgar indicated no relevant financial relationships.
Christopher Stallwood indicated no relevant financial relationships.
Helena Lau indicated no relevant financial relationships.
Yuxuan Jiang, BSc1, Kayla Dadgar, MD2, Christopher Stallwood, MD2, Helena Lau, MD, FRCPC3. P3517 - Development of Diffuse Upper Gastrointestinal Tract Submucosal Petechiae and Haemorrhage in a Patient With Newly Diagnosed Primary Immune Thrombocytopenic Purpura, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
