Tuesday Poster Session
Category: Esophagus
P3278 - Treatment of Bile Reflux Phenotype Improved Response to Treatment in PPI Refractory GERD Patients
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
- MT
Mumtaz Tabbaa, MD
Natividad Medical Center
Salinas, CA
Presenting Author(s)
Mumtaz Tabbaa, MD, Alex Di Stante, MD
Natividad Medical Center, Salinas, CA
Introduction: GERD has become a heterogeneous disorder with many phenotypes and etiologies requiring different managements. About 60% of GERD patients responded to PPI therapy, however the pathophysiology of PPI refractory GERD (R-GERD) remained controversial and unclear. Compiled evidence showed bile reflux could induce mucosal damage (1), Gastrin hormonal changes (2), and could be an important etiology of GERD. We aim in this study to assess the response to treatment of R-GERD patients when they received optimal therapy of combined anti-acid and anti-bile medications, based on the previously reported high prevalence of bile reflux in this group of patients (3).
Methods: This is a retrospective cohort study of 322 adult patients with R-GERD who were referred to the GI service of the county hospital between 2013 and 2022. Medical data extraction included demographics, past medical and surgical history, serum Gastrin, in addition to endoscopy data on all patients including the presence of bile liquid, and LA class of GERD. patients with H. Pylori, gastroparesis, gastric surgery, and ZE syndrome were excluded. All patients were treated with combination of acid suppression agent and protective coating agent (Sucralfate) for 6 weeks at least, which was considered as standard treatment for R-GERD in this GI practice. Response to treatment was defined as clinical remission of symptoms and endoscopic remission for LA class C, and D by repeated EGD.
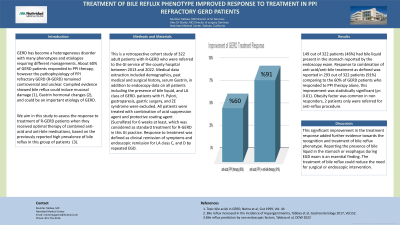
Results: 149 out of 322 patients (46%) had bile liquid present in the stomach reported by the endoscopy exam. Response to combination of anti-acid/anti-bile treatment as defined was reported in 293 out of 322 patients (91%) comparing to the 60% of GERD patients who responded to PPI therapy alone, this improvement was statistically significant (p< 0.01). Obesity factor was common in non responders, 2 patients only were referred for anti-reflux procedure.
Discussion: This significant improvement in the treatment response added further evidence towards the recognition and treatment of bile reflux phenotype. Reporting the presence of bile liquid in the stomach or esophagus during EGD exam is an essential finding. The treatment of bile reflux could reduce the need for surgical or endoscopic intervention.
References: (1) Toxic bile acids in GERD, Nehra et al, Gut 1999, Vol. 44. (2) Bile reflux increased the incidence of Hypergastrinemia, Tabbaa et al, Gastroenterology 2017, Vol. 152. (3) Bile reflux prediction by non endoscopic factors, Tabbaa et al, DDW 2022
Disclosures:
Mumtaz Tabbaa, MD, Alex Di Stante, MD. P3278 - Treatment of Bile Reflux Phenotype Improved Response to Treatment in PPI Refractory GERD Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Natividad Medical Center, Salinas, CA
Introduction: GERD has become a heterogeneous disorder with many phenotypes and etiologies requiring different managements. About 60% of GERD patients responded to PPI therapy, however the pathophysiology of PPI refractory GERD (R-GERD) remained controversial and unclear. Compiled evidence showed bile reflux could induce mucosal damage (1), Gastrin hormonal changes (2), and could be an important etiology of GERD. We aim in this study to assess the response to treatment of R-GERD patients when they received optimal therapy of combined anti-acid and anti-bile medications, based on the previously reported high prevalence of bile reflux in this group of patients (3).
Methods: This is a retrospective cohort study of 322 adult patients with R-GERD who were referred to the GI service of the county hospital between 2013 and 2022. Medical data extraction included demographics, past medical and surgical history, serum Gastrin, in addition to endoscopy data on all patients including the presence of bile liquid, and LA class of GERD. patients with H. Pylori, gastroparesis, gastric surgery, and ZE syndrome were excluded. All patients were treated with combination of acid suppression agent and protective coating agent (Sucralfate) for 6 weeks at least, which was considered as standard treatment for R-GERD in this GI practice. Response to treatment was defined as clinical remission of symptoms and endoscopic remission for LA class C, and D by repeated EGD.
Results: 149 out of 322 patients (46%) had bile liquid present in the stomach reported by the endoscopy exam. Response to combination of anti-acid/anti-bile treatment as defined was reported in 293 out of 322 patients (91%) comparing to the 60% of GERD patients who responded to PPI therapy alone, this improvement was statistically significant (p< 0.01). Obesity factor was common in non responders, 2 patients only were referred for anti-reflux procedure.
Discussion: This significant improvement in the treatment response added further evidence towards the recognition and treatment of bile reflux phenotype. Reporting the presence of bile liquid in the stomach or esophagus during EGD exam is an essential finding. The treatment of bile reflux could reduce the need for surgical or endoscopic intervention.
References: (1) Toxic bile acids in GERD, Nehra et al, Gut 1999, Vol. 44. (2) Bile reflux increased the incidence of Hypergastrinemia, Tabbaa et al, Gastroenterology 2017, Vol. 152. (3) Bile reflux prediction by non endoscopic factors, Tabbaa et al, DDW 2022
Disclosures:
Mumtaz Tabbaa indicated no relevant financial relationships.
Alex Di Stante indicated no relevant financial relationships.
Mumtaz Tabbaa, MD, Alex Di Stante, MD. P3278 - Treatment of Bile Reflux Phenotype Improved Response to Treatment in PPI Refractory GERD Patients, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
