Tuesday Poster Session
Category: Esophagus
P3284 - Pseudoachalasia - An Uncoventional Method of Diagnosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- AD
Anand Dwivedi, MD
Carilion Clinic
Roanoke, Virginia
Presenting Author(s)
Anand Dwivedi, MD, Raj Shah, MD
Carilion Clinic, Roanoke, VA
Introduction: In pseudoachalasia, radiographic and manometric features of achalasia do not typically reveal the underlying pathology. Pseudoachalasia due to malignancy, most commonly in the gastric cardia, is responsible for approximately 5% of cases with manometric findings suggestive of achalasia. We present a case of an elderly female with a 2 year history of dysphagia and manometric findings suggestive of esophagogastric junction outflow obstruction (EGJOO).
Case Description/Methods: An elderly female with a history of breast cancer in remission presents with complaints of mild esophageal dysphagia and persistent reflux. Index EGD was normal, with empiric 52 French Maloney dilation. Dysphagia persisted, hence repeat EGD was performed several months later with a mild stricture was noted at the GE junction. 54 French Maloney dilation was performed. Manometry demonstrated an elevated integrated relaxation pressure (IRP) of 31.7 mm Hg, suggestive of EGJOO. She was suggested to undergo a trial of GE junction Botox injection given concern for achalasia. Esophagram performed prior to Botox injection showed tablet arrest at the GE junction with liquid contrast material filtering around the pill into the stomach with no evidence of stricture or mass at the GE junction. There was endoscopically evident GE junction relaxation after Botox injection. Heller myotomy was pursued. During laparoscopic examination, the upper portion of the stomach was noted to be immobile. Intraoperative endoscopy was used to evaluate the GE junction, with multiple biopsies taken, revealing highly atypical cells at basilar aspects of few consecutive glands within the lamina propria. Endoscopic ultrasound (EUS) was then pursued, showing distal esophageal wall thickening and cardia wall thickening along with muscularis propria thickening on EUS. Multiple bite on bite biopsies were taken of the lower esophagus and cardia, with biopsies demonstrating metastatic breast carcinoma.
Discussion: Numerous endoscopic evaluations were completed without suspicion for pseudoachalasia. Only gross anatomic examination of the cardia and upper portion of the stomach during surgery raised suspicion for malignancy. This case raises the question of whether empiric biopsies should be taken from the GE junction in all new cases of achalasia. It also begs the question of the role of EUS in evaluating pseudoachalasia in new cases of achalasia in the elderly.

Disclosures:
Anand Dwivedi, MD, Raj Shah, MD. P3284 - Pseudoachalasia - An Uncoventional Method of Diagnosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Carilion Clinic, Roanoke, VA
Introduction: In pseudoachalasia, radiographic and manometric features of achalasia do not typically reveal the underlying pathology. Pseudoachalasia due to malignancy, most commonly in the gastric cardia, is responsible for approximately 5% of cases with manometric findings suggestive of achalasia. We present a case of an elderly female with a 2 year history of dysphagia and manometric findings suggestive of esophagogastric junction outflow obstruction (EGJOO).
Case Description/Methods: An elderly female with a history of breast cancer in remission presents with complaints of mild esophageal dysphagia and persistent reflux. Index EGD was normal, with empiric 52 French Maloney dilation. Dysphagia persisted, hence repeat EGD was performed several months later with a mild stricture was noted at the GE junction. 54 French Maloney dilation was performed. Manometry demonstrated an elevated integrated relaxation pressure (IRP) of 31.7 mm Hg, suggestive of EGJOO. She was suggested to undergo a trial of GE junction Botox injection given concern for achalasia. Esophagram performed prior to Botox injection showed tablet arrest at the GE junction with liquid contrast material filtering around the pill into the stomach with no evidence of stricture or mass at the GE junction. There was endoscopically evident GE junction relaxation after Botox injection. Heller myotomy was pursued. During laparoscopic examination, the upper portion of the stomach was noted to be immobile. Intraoperative endoscopy was used to evaluate the GE junction, with multiple biopsies taken, revealing highly atypical cells at basilar aspects of few consecutive glands within the lamina propria. Endoscopic ultrasound (EUS) was then pursued, showing distal esophageal wall thickening and cardia wall thickening along with muscularis propria thickening on EUS. Multiple bite on bite biopsies were taken of the lower esophagus and cardia, with biopsies demonstrating metastatic breast carcinoma.
Discussion: Numerous endoscopic evaluations were completed without suspicion for pseudoachalasia. Only gross anatomic examination of the cardia and upper portion of the stomach during surgery raised suspicion for malignancy. This case raises the question of whether empiric biopsies should be taken from the GE junction in all new cases of achalasia. It also begs the question of the role of EUS in evaluating pseudoachalasia in new cases of achalasia in the elderly.

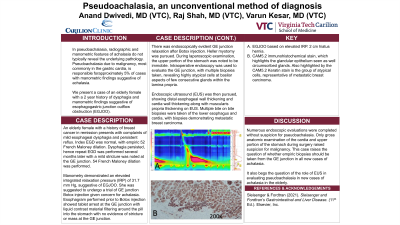
Figure: A: EGJOO based on elevated IRP. 2 cm hiatus hernia.
B: CAM5.2 immunohistochemical stain, which highlights the glandular epithelium seen as well circumscribed glands. Also highlighted by the CAM5.2 keratin stain is the group of atypical cells, representative of metastatic breast carcinoma.
B: CAM5.2 immunohistochemical stain, which highlights the glandular epithelium seen as well circumscribed glands. Also highlighted by the CAM5.2 keratin stain is the group of atypical cells, representative of metastatic breast carcinoma.
Disclosures:
Anand Dwivedi indicated no relevant financial relationships.
Raj Shah indicated no relevant financial relationships.
Anand Dwivedi, MD, Raj Shah, MD. P3284 - Pseudoachalasia - An Uncoventional Method of Diagnosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
