Tuesday Poster Session
Category: Esophagus
P3286 - Mallory-Weiss Syndrome Marked by Sporadic Hematemesis and Extensive Clots
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Seth Lipshutz, DO
Jefferson Health Northeast
Philadelphia, PA
Presenting Author(s)
Seth Lipshutz, DO1, Parmjyot Singh, DO2, Jessica A.. Schumann, DO1
1Jefferson Health Northeast, Philadelphia, PA; 2Jefferson Health, Philadelphia, PA
Introduction: The reported incidence of Mallory-Weiss syndrome among patients presenting with upper gastrointestinal bleeding ranges from 8 to 15%. It is likely that Mallory-Weiss syndrome occurs in a less severe form more frequently than is recognized. The pathogenesis of Mallory-Weiss Syndrome has yet to be completely understood. It has been proposed that mucosal lacerations develop secondary to a sudden increase in intra-abdominal pressure. We present a case of Mallory-Weiss Syndrome that initially presented with concern for malignancy due to clot formation.
Case Description/Methods: A 75-year-old female with a history of gastroesophageal reflux (GERD) presented for acute dysphagia and odynophagia evaluation. Her exam revealed brown residue in the oral cavity and epigastric abdominal tenderness. Neck imaging revealed thickening of the posterior wall of the left piriform sinus and aryepiglottic fold and a 17 x 3.4 cm mass at the gastroesophageal junction. We entertained the idea of malignancy due to the mass. Her course was complicated by profound hematemesis, hematochezia, and hemodynamic instability marked by uncontrolled atrial fibrillation. This prompted a transfer to the ICU and an emergent esophagogastroduodenoscopy (EGD) devoid of active bleeding. A subsequent EGD demonstrated extensive esophagitis, and clots transverse the entire esophagus, also seen on the first scope. A third EGD, performed at the nadir of her stay, confirmed a sizable Mallory Weiss tear in the healing stage. Biopsies were negative for malignant cells, and the patient was discharged home.
Discussion: Mallory-Weiss Syndrome can present with vomiting and hematemesis, which may range from light streaks of blood to large-volume hemorrhage and epigastric pain, which may radiate to the back. Recognizing the anatomical area referred to by this syndrome, standard differentials include other esophageal pathology. The gold standard for evaluation and diagnosis is by EGD. CT angiography is helpful when EGD is unavailable or there is active bleeding without precise endoscopic localization.

Disclosures:
Seth Lipshutz, DO1, Parmjyot Singh, DO2, Jessica A.. Schumann, DO1. P3286 - Mallory-Weiss Syndrome Marked by Sporadic Hematemesis and Extensive Clots, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Jefferson Health Northeast, Philadelphia, PA; 2Jefferson Health, Philadelphia, PA
Introduction: The reported incidence of Mallory-Weiss syndrome among patients presenting with upper gastrointestinal bleeding ranges from 8 to 15%. It is likely that Mallory-Weiss syndrome occurs in a less severe form more frequently than is recognized. The pathogenesis of Mallory-Weiss Syndrome has yet to be completely understood. It has been proposed that mucosal lacerations develop secondary to a sudden increase in intra-abdominal pressure. We present a case of Mallory-Weiss Syndrome that initially presented with concern for malignancy due to clot formation.
Case Description/Methods: A 75-year-old female with a history of gastroesophageal reflux (GERD) presented for acute dysphagia and odynophagia evaluation. Her exam revealed brown residue in the oral cavity and epigastric abdominal tenderness. Neck imaging revealed thickening of the posterior wall of the left piriform sinus and aryepiglottic fold and a 17 x 3.4 cm mass at the gastroesophageal junction. We entertained the idea of malignancy due to the mass. Her course was complicated by profound hematemesis, hematochezia, and hemodynamic instability marked by uncontrolled atrial fibrillation. This prompted a transfer to the ICU and an emergent esophagogastroduodenoscopy (EGD) devoid of active bleeding. A subsequent EGD demonstrated extensive esophagitis, and clots transverse the entire esophagus, also seen on the first scope. A third EGD, performed at the nadir of her stay, confirmed a sizable Mallory Weiss tear in the healing stage. Biopsies were negative for malignant cells, and the patient was discharged home.
Discussion: Mallory-Weiss Syndrome can present with vomiting and hematemesis, which may range from light streaks of blood to large-volume hemorrhage and epigastric pain, which may radiate to the back. Recognizing the anatomical area referred to by this syndrome, standard differentials include other esophageal pathology. The gold standard for evaluation and diagnosis is by EGD. CT angiography is helpful when EGD is unavailable or there is active bleeding without precise endoscopic localization.

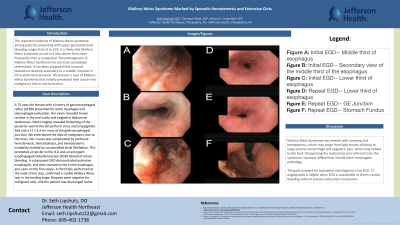
Figure: A. Initial EGD-- Middle third of esophagus
B. Initial EGD-- Secondary view of the middle third of the esophagus
C. Initial EGD-- Lower third of esophagus
D. Repeat EGD-- Lower third of esophagus
E. Repeat EGD-- GE Junction
F. Repeat EGD-- Stomach Fundus
B. Initial EGD-- Secondary view of the middle third of the esophagus
C. Initial EGD-- Lower third of esophagus
D. Repeat EGD-- Lower third of esophagus
E. Repeat EGD-- GE Junction
F. Repeat EGD-- Stomach Fundus
Disclosures:
Seth Lipshutz indicated no relevant financial relationships.
Parmjyot Singh indicated no relevant financial relationships.
Jessica Schumann indicated no relevant financial relationships.
Seth Lipshutz, DO1, Parmjyot Singh, DO2, Jessica A.. Schumann, DO1. P3286 - Mallory-Weiss Syndrome Marked by Sporadic Hematemesis and Extensive Clots, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
