Tuesday Poster Session
Category: Esophagus
P3292 - Pseudoachalasia Secondary to Esophageal Leiomyomatosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Shefali Amin, DO, MSEd
Reading Hospital
Reading, PA
Presenting Author(s)
Iman Khan, MD1, Hira Hanif, MD1, Shefali Amin, DO, MSEd2, Jesus Salas Noain, MD1, John Altomare, MD1, Nirav Shah, MD1
1Reading Hospital Tower Health, Reading, PA; 2Reading Hospital, Reading, PA
Introduction: Leiomyomas represent less than 1 % of esophageal neoplasms yet constitute 67% of the benign esophageal tumors. These may be single or multiple, generally presenting most frequently between ages 20-50 with dysphagia. They are usually slow growing tumors; however, giant leiomyomas can grow rapidly. The mainstay of treatment is resection or enucleation by conventional thoracotomy or thoracoscopy. However, for giant symptomatic esophageal leiomyomas, esophagectomy remains an option.
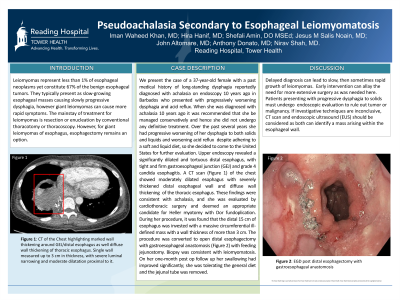
Case Description/Methods: We present the case of a 37-year-old female with a past medical history of long-standing dysphagia reportedly diagnosed with achalasia on endoscopy 10 years ago in Barbados who presented with progressively worsening dysphagia and regurgitation. She was being managed conservatively with soft, liquid diet. Over the past several years she had progressive worsening of her dysphagia, to both solids and liquids, despite adhering to a soft diet so she decided to come to the for treatment. She underwent an upper endoscopy which revealed a significantly dilated and tortuous distal esophagus, with tight gastroesophageal junction (GEJ) and grade 4 candida esophagitis. This was followed by a CT scan of the chest that showed moderately dilated esophagus with severely thickened distal esophageal wall and diffuse wall thickenings across thoracic esophagus. These findings were consistent with achalasia, and she was evaluated by cardiothoracic surgery and deemed an appropriate candidate for Heller myotomy with Dor fundoplication. Shockingly during her procedure, it was found that the distal 15 cm of esophagus was invested with a massive circumferential ill-defined mass with a wall thickness of more than 3 cm. The procedure was converted to open distal esophagectomy with gastroesophageal anastomosis with feeding jejunostomy. Biopsy was consistent with leiomyomatosis. On her one-month post op follow up her swallowing had improved significantly; she was tolerating the general diet and the jejunal tube was removed.
Discussion: Delayed diagnosis can lead to slow and then rapid growth of leiomyomas leading to more aggressive treatment routes, as observed in this case, where the patient required esophagectomy. Patients presenting with progressive dysphagia to solids must undergo evaluation to rule out tumor or malignancy. If endoscopy and barium study are inconclusive, CT scan and endoscopic ultrasound (EUS) should be considered as both can highlight uniform density of the mass arising within the esophageal wall.

Disclosures:
Iman Khan, MD1, Hira Hanif, MD1, Shefali Amin, DO, MSEd2, Jesus Salas Noain, MD1, John Altomare, MD1, Nirav Shah, MD1. P3292 - Pseudoachalasia Secondary to Esophageal Leiomyomatosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Reading Hospital Tower Health, Reading, PA; 2Reading Hospital, Reading, PA
Introduction: Leiomyomas represent less than 1 % of esophageal neoplasms yet constitute 67% of the benign esophageal tumors. These may be single or multiple, generally presenting most frequently between ages 20-50 with dysphagia. They are usually slow growing tumors; however, giant leiomyomas can grow rapidly. The mainstay of treatment is resection or enucleation by conventional thoracotomy or thoracoscopy. However, for giant symptomatic esophageal leiomyomas, esophagectomy remains an option.
Case Description/Methods: We present the case of a 37-year-old female with a past medical history of long-standing dysphagia reportedly diagnosed with achalasia on endoscopy 10 years ago in Barbados who presented with progressively worsening dysphagia and regurgitation. She was being managed conservatively with soft, liquid diet. Over the past several years she had progressive worsening of her dysphagia, to both solids and liquids, despite adhering to a soft diet so she decided to come to the for treatment. She underwent an upper endoscopy which revealed a significantly dilated and tortuous distal esophagus, with tight gastroesophageal junction (GEJ) and grade 4 candida esophagitis. This was followed by a CT scan of the chest that showed moderately dilated esophagus with severely thickened distal esophageal wall and diffuse wall thickenings across thoracic esophagus. These findings were consistent with achalasia, and she was evaluated by cardiothoracic surgery and deemed an appropriate candidate for Heller myotomy with Dor fundoplication. Shockingly during her procedure, it was found that the distal 15 cm of esophagus was invested with a massive circumferential ill-defined mass with a wall thickness of more than 3 cm. The procedure was converted to open distal esophagectomy with gastroesophageal anastomosis with feeding jejunostomy. Biopsy was consistent with leiomyomatosis. On her one-month post op follow up her swallowing had improved significantly; she was tolerating the general diet and the jejunal tube was removed.
Discussion: Delayed diagnosis can lead to slow and then rapid growth of leiomyomas leading to more aggressive treatment routes, as observed in this case, where the patient required esophagectomy. Patients presenting with progressive dysphagia to solids must undergo evaluation to rule out tumor or malignancy. If endoscopy and barium study are inconclusive, CT scan and endoscopic ultrasound (EUS) should be considered as both can highlight uniform density of the mass arising within the esophageal wall.

Figure: Barium esophagram showing narrowing of the distal esophagus with dilation of the mid and proximal esophagus
Disclosures:
Iman Khan indicated no relevant financial relationships.
Hira Hanif indicated no relevant financial relationships.
Shefali Amin indicated no relevant financial relationships.
Jesus Salas Noain indicated no relevant financial relationships.
John Altomare indicated no relevant financial relationships.
Nirav Shah indicated no relevant financial relationships.
Iman Khan, MD1, Hira Hanif, MD1, Shefali Amin, DO, MSEd2, Jesus Salas Noain, MD1, John Altomare, MD1, Nirav Shah, MD1. P3292 - Pseudoachalasia Secondary to Esophageal Leiomyomatosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
