Tuesday Poster Session
Category: Esophagus
P3293 - An Unusual Cause of Dysphagia
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
John Ko, DO
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
John Ko, DO1, Rebecca Salvo, DO1, Jeevin Sandhu, 2, Vishvinder Sharma, MD1
1Valley Hospital Medical Center, Las Vegas, NV; 2Tour University Nevada, Henderson, NV
Introduction: The causes and differential diagnoses for dysphagia are broad and diagnostic approaches vary. Characterizing symptoms, occurrence with solids and/or liquids, and acuteness are important. Dysphagia may stem from structural abnormalities causing obstruction or narrowing or due to motility abnormalities. Endoscopy is often warranted as part of the work up and this case demonstrates the importance of direct visualization.
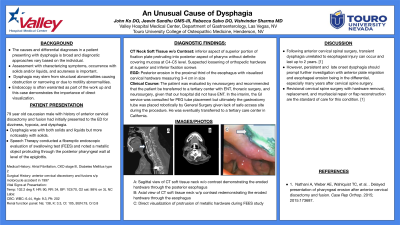
Case Description/Methods: 79-year-old male with PMH atrial fibrillation, CKD Stage 3, diabetes, and neck surgeries including an anterior cervical discectomy and fusion after a motorcycle accident in 1997 initially presented to our institution with dizziness and dysphagia. He described a choking sensation with swallowing. He felt he could not coordinate swallowing both liquids and solids and as if solids would get stuck. While in the hospital he started to not be able to tolerate his own secretions and required suctioning. Speech therapy was consulted and performed a fiberoptic endoscopic evaluation of swallowing test and saw a metallic object along the posterior pharyngeal wall at the level of the epiglottis. The posterior pharyngeal wall was protruding into the pharynx with limited space between the epiglottis and posterior pharyngeal wall. During the test, the patient demonstrated reduced laryngeal elevation and epiglottic inversion with penetration to the level of the vocal cords. CT neck soft tissue without contrast demonstrated an inferior active aspect of the superior portion of the fixation plate protruding into the posterior aspect of the pharynx without definitive covering mucosa at approximately the level of C4-5 level. GI was consulted for PEG placement given inability to swallow and need for ongoing nutrition. Upon EGD, there was again noted metal protruding though the posterior pharynx, as well as an erosion of hardware in the proximal third of the esophagus. A gastrostomy tube was placed endoscopically for ongoing nutrition.
Discussion: Few case reports have had similar presentations. Following anterior cervical spinal surgery, transient dysphagia unrelated to esophageal injury can occur and last up to 2 years but late onset dysphagia warrants further investigation. Anterior migration and esophageal migration must be in the differential, especially years after cervical spine surgery. Revisional cervical spine surgery with hardware removal, replacement, and myofascial repair or flap reconstruction are the standard of care for this condition.

Disclosures:
John Ko, DO1, Rebecca Salvo, DO1, Jeevin Sandhu, 2, Vishvinder Sharma, MD1. P3293 - An Unusual Cause of Dysphagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Valley Hospital Medical Center, Las Vegas, NV; 2Tour University Nevada, Henderson, NV
Introduction: The causes and differential diagnoses for dysphagia are broad and diagnostic approaches vary. Characterizing symptoms, occurrence with solids and/or liquids, and acuteness are important. Dysphagia may stem from structural abnormalities causing obstruction or narrowing or due to motility abnormalities. Endoscopy is often warranted as part of the work up and this case demonstrates the importance of direct visualization.
Case Description/Methods: 79-year-old male with PMH atrial fibrillation, CKD Stage 3, diabetes, and neck surgeries including an anterior cervical discectomy and fusion after a motorcycle accident in 1997 initially presented to our institution with dizziness and dysphagia. He described a choking sensation with swallowing. He felt he could not coordinate swallowing both liquids and solids and as if solids would get stuck. While in the hospital he started to not be able to tolerate his own secretions and required suctioning. Speech therapy was consulted and performed a fiberoptic endoscopic evaluation of swallowing test and saw a metallic object along the posterior pharyngeal wall at the level of the epiglottis. The posterior pharyngeal wall was protruding into the pharynx with limited space between the epiglottis and posterior pharyngeal wall. During the test, the patient demonstrated reduced laryngeal elevation and epiglottic inversion with penetration to the level of the vocal cords. CT neck soft tissue without contrast demonstrated an inferior active aspect of the superior portion of the fixation plate protruding into the posterior aspect of the pharynx without definitive covering mucosa at approximately the level of C4-5 level. GI was consulted for PEG placement given inability to swallow and need for ongoing nutrition. Upon EGD, there was again noted metal protruding though the posterior pharynx, as well as an erosion of hardware in the proximal third of the esophagus. A gastrostomy tube was placed endoscopically for ongoing nutrition.
Discussion: Few case reports have had similar presentations. Following anterior cervical spinal surgery, transient dysphagia unrelated to esophageal injury can occur and last up to 2 years but late onset dysphagia warrants further investigation. Anterior migration and esophageal migration must be in the differential, especially years after cervical spine surgery. Revisional cervical spine surgery with hardware removal, replacement, and myofascial repair or flap reconstruction are the standard of care for this condition.

Figure: Erosion of Hardware Through the Posterior Pharynx
Disclosures:
John Ko indicated no relevant financial relationships.
Rebecca Salvo indicated no relevant financial relationships.
Jeevin Sandhu indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
John Ko, DO1, Rebecca Salvo, DO1, Jeevin Sandhu, 2, Vishvinder Sharma, MD1. P3293 - An Unusual Cause of Dysphagia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
