Tuesday Poster Session
Category: Small Intestine
P4178 - A Case of Lactobacillus Bacteremia in a Patient on Chronic Total Parenteral Nutrition
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Hannah W. Fiske, MD
Brown University/Rhode Island Hospital
Providence, RI
Presenting Author(s)
Hannah W. Fiske, MD1, Breton Roussel, MD2, Marion Winkler, RD, PhD3, Benjamin M. Hall, MD4
1Brown University/Rhode Island Hospital, Providence, RI; 2Brown University, Providence, RI; 3Rhode Island Hospital, Brown University Medical School, Providence, RI; 4Brown Surgical Associates, Providence, RI
Introduction: Short bowel syndrome (SBS) is a condition caused by the physical loss of a portion of the intestine, whereafter the body is subsequently unable to adequately absorb nutrients, fluids, and electrolytes. The remnant colon and its microbiota significantly impact patient outcomes; SBS has high levels of morbidity and mortality. Patients with SBS have an altered gut microbiome, with reduced bacterial diversity and high prevalence of lactobacillus; this is exacerbated in patients with severe disease or requiring total parenteral nutrition (TPN). Here we describe a case of a patient with SBS on chronic TPN who developed lactobacillus bacteremia, believed to be an atypical line infection of her chronic peripherally inserted central catheter (PICC).
Case Description/Methods: A 60-year-old female presented with chest pain. Past surgical history was significant for appendectomy with cecectomy complicated by retroperitoneal abscess, internal hernia and subsequent small bowel resection, and right and transverse colon resection with end ileostomy. She experienced intestinal failure secondary to SBS (115cm remnant small intestine) and had been placed on chronic TPN via PICC. Abdominal exam on admission was unremarkable, and she denied abdominal pain or changes in bowel function.
Imaging was notable for PICC-associated DVT, for which anticoagulation was started. During hospitalization she developed severe abdominal pain and decreased frequency of bowel movements. Abdominal CT revealed chronic stable intestinal distension without discrete transition point (Figure 1). Blood cultures from her PICC and peripheral IV ultimately grew lactobacillus. Her PICC was removed; blood cultures normalized after initiation of broad-spectrum antibiotics.
Discussion: Lactobacillus is a ubiquitous microorganism that most frequently colonizes mucosal surfaces such as the GI tract. Though generally considered beneficial, an over-abundance of lactobacilli with resulting bacterial imbalance can exacerbate malabsorption and cause GI symptoms. Lactobacillus bacteremia is rare with limited occurrence in current medical literature. Given its known tendency to colonize the GI tract, it has been linked to polymicrobial infections stemming from a GI source.
The lactobacillus bacteremia described here was determined to be a PICC infection. Given her concomitant abdominal symptoms and extensive history of surgical manipulation, the more likely presumed diagnosis would have been from an intraabdominal source.

Disclosures:
Hannah W. Fiske, MD1, Breton Roussel, MD2, Marion Winkler, RD, PhD3, Benjamin M. Hall, MD4. P4178 - A Case of Lactobacillus Bacteremia in a Patient on Chronic Total Parenteral Nutrition, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Brown University/Rhode Island Hospital, Providence, RI; 2Brown University, Providence, RI; 3Rhode Island Hospital, Brown University Medical School, Providence, RI; 4Brown Surgical Associates, Providence, RI
Introduction: Short bowel syndrome (SBS) is a condition caused by the physical loss of a portion of the intestine, whereafter the body is subsequently unable to adequately absorb nutrients, fluids, and electrolytes. The remnant colon and its microbiota significantly impact patient outcomes; SBS has high levels of morbidity and mortality. Patients with SBS have an altered gut microbiome, with reduced bacterial diversity and high prevalence of lactobacillus; this is exacerbated in patients with severe disease or requiring total parenteral nutrition (TPN). Here we describe a case of a patient with SBS on chronic TPN who developed lactobacillus bacteremia, believed to be an atypical line infection of her chronic peripherally inserted central catheter (PICC).
Case Description/Methods: A 60-year-old female presented with chest pain. Past surgical history was significant for appendectomy with cecectomy complicated by retroperitoneal abscess, internal hernia and subsequent small bowel resection, and right and transverse colon resection with end ileostomy. She experienced intestinal failure secondary to SBS (115cm remnant small intestine) and had been placed on chronic TPN via PICC. Abdominal exam on admission was unremarkable, and she denied abdominal pain or changes in bowel function.
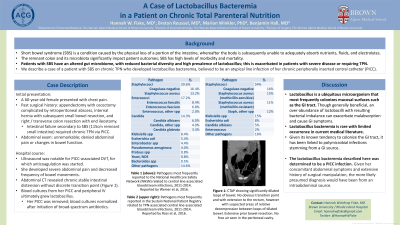
Imaging was notable for PICC-associated DVT, for which anticoagulation was started. During hospitalization she developed severe abdominal pain and decreased frequency of bowel movements. Abdominal CT revealed chronic stable intestinal distension without discrete transition point (Figure 1). Blood cultures from her PICC and peripheral IV ultimately grew lactobacillus. Her PICC was removed; blood cultures normalized after initiation of broad-spectrum antibiotics.
Discussion: Lactobacillus is a ubiquitous microorganism that most frequently colonizes mucosal surfaces such as the GI tract. Though generally considered beneficial, an over-abundance of lactobacilli with resulting bacterial imbalance can exacerbate malabsorption and cause GI symptoms. Lactobacillus bacteremia is rare with limited occurrence in current medical literature. Given its known tendency to colonize the GI tract, it has been linked to polymicrobial infections stemming from a GI source.
The lactobacillus bacteremia described here was determined to be a PICC infection. Given her concomitant abdominal symptoms and extensive history of surgical manipulation, the more likely presumed diagnosis would have been from an intraabdominal source.

Figure: Figure 1: CTAP, coronal (a) and axial (b) slices, showing significantly dilated loops of bowel, in various configurations, progressed relative to prior imaging. No obvious transition point and with extension to the rectum, however with suspected areas of relative decompression between loops of dilated bowel. Extensive prior bowel resection. No free air seen in the peritoneal cavity.
Disclosures:
Hannah Fiske indicated no relevant financial relationships.
Breton Roussel indicated no relevant financial relationships.
Marion Winkler: Takeda Pharmaceutical – Consultant. VectivBio – Advisor or Review Panel Member, Consultant.
Benjamin Hall indicated no relevant financial relationships.
Hannah W. Fiske, MD1, Breton Roussel, MD2, Marion Winkler, RD, PhD3, Benjamin M. Hall, MD4. P4178 - A Case of Lactobacillus Bacteremia in a Patient on Chronic Total Parenteral Nutrition, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
