Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3182 - Adenoma Detection Rate Tracking Simplified: Tableau-Based Automated Quality Dashboard
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Melinda Wang, MD, MHS
University of California San Francisco
San Francisco, CA
Presenting Author(s)
Melinda Wang, MD, MHS1, Aris Oates, MD1, Aparajita Singh, MD, MPH2
1University of California San Francisco, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA
Introduction: Adenoma detection rate (ADR), defined as the proportion of screening colonoscopies performed by a physician with ≥1 identified adenoma, is a key quality indicator of colonoscopy that is inversely associated with post-colonoscopy colon cancer risk. Measuring ADR, however, requires manual data abstraction and collating asynchronous pathology/procedural reports from multiple sources via third party software or national registry which require significant time and cost. Several institutions have used natural language processing (NLP) to develop ADR tools, however, few institutions have successfully developed fully automated ADR dashboards. We sought to develop a fully automated colonoscopy Quality Improvement (QI) reporting system without manual data abstraction or change in physician workflow.
Methods: At our institution, endoscopy reports written in Endopro software are pushed to the electronic medical record, EPIC. With NLP, free text colonoscopy and pathology reports were processed with extraction of patient demographic and procedure data. Using the data visualization tool, Tableau, data was presented as a dashboard for display and filtering. Manual validation of metrics was done to ensure accuracy of NLP classifications.
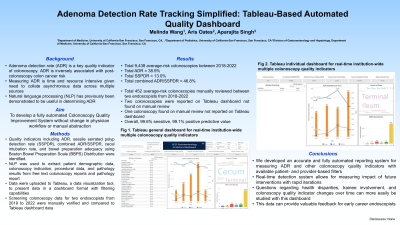
Results: This dashboard reports institution-wide colonoscopy QI indicators including type, ADR, serrated polyp detection rate, bowel preparation adequacy, and cecal intubation rate (Figure 1). Data from 2019 onwards are available at an aggregated and individual physician level. The dashboard can track ADR for screening vs other indication by physician, addressing the issue of potentially “gaming” the ADR. Multiple filters can be applied to visualize how QI indicators are impacted by trainee involvement, language, age, gender, race/ethnicity, and BMI. ADR evolution of a given physician over time can be tracked, which can be of value for early career endoscopists. The QI dashboard was 100% accurate in capturing data and reporting QI indicators during extensive data validation process with manual data review.
Discussion: We developed an accurate and fully automated reporting system for measuring ADR and other colonoscopy QI indicators that provides individual patient- and physician- based filters. This dashboard does not require changes to physician workflow or manual data abstraction. Other institutions looking to create a similar dashboard should ensure the NLP used to define metrics are validated and accurate.

Disclosures:
Melinda Wang, MD, MHS1, Aris Oates, MD1, Aparajita Singh, MD, MPH2. P3182 - Adenoma Detection Rate Tracking Simplified: Tableau-Based Automated Quality Dashboard, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of California San Francisco, San Francisco, CA; 2University of California, San Francisco, San Francisco, CA
Introduction: Adenoma detection rate (ADR), defined as the proportion of screening colonoscopies performed by a physician with ≥1 identified adenoma, is a key quality indicator of colonoscopy that is inversely associated with post-colonoscopy colon cancer risk. Measuring ADR, however, requires manual data abstraction and collating asynchronous pathology/procedural reports from multiple sources via third party software or national registry which require significant time and cost. Several institutions have used natural language processing (NLP) to develop ADR tools, however, few institutions have successfully developed fully automated ADR dashboards. We sought to develop a fully automated colonoscopy Quality Improvement (QI) reporting system without manual data abstraction or change in physician workflow.
Methods: At our institution, endoscopy reports written in Endopro software are pushed to the electronic medical record, EPIC. With NLP, free text colonoscopy and pathology reports were processed with extraction of patient demographic and procedure data. Using the data visualization tool, Tableau, data was presented as a dashboard for display and filtering. Manual validation of metrics was done to ensure accuracy of NLP classifications.
Results: This dashboard reports institution-wide colonoscopy QI indicators including type, ADR, serrated polyp detection rate, bowel preparation adequacy, and cecal intubation rate (Figure 1). Data from 2019 onwards are available at an aggregated and individual physician level. The dashboard can track ADR for screening vs other indication by physician, addressing the issue of potentially “gaming” the ADR. Multiple filters can be applied to visualize how QI indicators are impacted by trainee involvement, language, age, gender, race/ethnicity, and BMI. ADR evolution of a given physician over time can be tracked, which can be of value for early career endoscopists. The QI dashboard was 100% accurate in capturing data and reporting QI indicators during extensive data validation process with manual data review.
Discussion: We developed an accurate and fully automated reporting system for measuring ADR and other colonoscopy QI indicators that provides individual patient- and physician- based filters. This dashboard does not require changes to physician workflow or manual data abstraction. Other institutions looking to create a similar dashboard should ensure the NLP used to define metrics are validated and accurate.

Figure: Real-time institution-wide colonoscopy QI indicators dashboard
Disclosures:
Melinda Wang indicated no relevant financial relationships.
Aris Oates indicated no relevant financial relationships.
Aparajita Singh indicated no relevant financial relationships.
Melinda Wang, MD, MHS1, Aris Oates, MD1, Aparajita Singh, MD, MPH2. P3182 - Adenoma Detection Rate Tracking Simplified: Tableau-Based Automated Quality Dashboard, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
