Tuesday Poster Session
Category: Colon
P3062 - Large Bowel Obstruction From Intraabdominal Mesh Masquerading as Toxic Megacolon
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- RF
Rhea Fogla, MD
New York-Presbyterian/Weill Cornell
New York, New York
Presenting Author(s)
Rhea Fogla, MD1, Aiya Aboubakr, MD2, David Wan, BS, MD3
1New York-Presbyterian/Weill Cornell, New York, NY; 2New York Presbyterian-Weill Cornell Medical Center, New York, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Toxic megacolon (TM) is a rare and potentially fatal complication that is characterized by nonobstructive colonic dilatation (greater than 6 cm diameter on radiographic film) with signs of systemic toxicity. There is a broad differential for colonic dilatation, though typically signs of toxicity can help differentiate TM from other conditions.
Case Description/Methods: An 80-year-old female with history of aortic stenosis status post valve replacement, polymyalgia rheumatica, breast cancer status post mastectomy, incisional hernia status post mesh repair, and IgA nephropathy presented to the hospital with acute lower abdominal pain. Labs were notable for a white blood cell count 36 x 103 µL, lactate 5.10 mmol/L and creatinine 3.34 mg/dL (baseline 1.7-2.0 mg/dL). Imaging revealed diffuse dilatation of the colon up to 8.5 cm and marked pericolonic inflammatory changes. Given concern for toxic megacolon, patient was initiated on broad spectrum antibiotics, including empiric C. difficile therapy. She underwent an exploratory laparotomy, which showed patchy necrosis throughout the ascending and transverse colon and a large bowel obstruction at the level of the intrabdominal mesh, resulting in subtotal colectomy with ileostomy. Stool sample tested negative for C. difficile. Post operatively, patient had increased pressor requirement despite resuscitation efforts. On exam, her ostomy site had a dusky appearance, which prompted an emergent exploratory laparotomy at bedside and resection of an ischemic end ileostomy. Surgical team planned to re-explore abdomen, however her family opted for comfort care and patient expired.
Discussion: Meeting diagnostic criteria for toxic megacolon is not definitive and does not preclude a patient from other etiologies of dilatation. As reflected in this case, large bowel obstructions can present with bowel necrosis and therefore lead to systemic toxicity, presenting in a similar fashion to TM. Identifying a patient’s clinical history and risk factors are critical, such as history of inflammatory bowel disease, clostridium difficile infection, and abdominal surgery. Given this patient’s significant clinical deterioration with worsening sepsis and end organ damage, surgical intervention was indicated regardless of etiology, as there is a high risk of bowel ischemia and perforation in both TM and bowel obstruction.

Disclosures:
Rhea Fogla, MD1, Aiya Aboubakr, MD2, David Wan, BS, MD3. P3062 - Large Bowel Obstruction From Intraabdominal Mesh Masquerading as Toxic Megacolon, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1New York-Presbyterian/Weill Cornell, New York, NY; 2New York Presbyterian-Weill Cornell Medical Center, New York, NY; 3Weill Cornell Medicine, New York, NY
Introduction: Toxic megacolon (TM) is a rare and potentially fatal complication that is characterized by nonobstructive colonic dilatation (greater than 6 cm diameter on radiographic film) with signs of systemic toxicity. There is a broad differential for colonic dilatation, though typically signs of toxicity can help differentiate TM from other conditions.
Case Description/Methods: An 80-year-old female with history of aortic stenosis status post valve replacement, polymyalgia rheumatica, breast cancer status post mastectomy, incisional hernia status post mesh repair, and IgA nephropathy presented to the hospital with acute lower abdominal pain. Labs were notable for a white blood cell count 36 x 103 µL, lactate 5.10 mmol/L and creatinine 3.34 mg/dL (baseline 1.7-2.0 mg/dL). Imaging revealed diffuse dilatation of the colon up to 8.5 cm and marked pericolonic inflammatory changes. Given concern for toxic megacolon, patient was initiated on broad spectrum antibiotics, including empiric C. difficile therapy. She underwent an exploratory laparotomy, which showed patchy necrosis throughout the ascending and transverse colon and a large bowel obstruction at the level of the intrabdominal mesh, resulting in subtotal colectomy with ileostomy. Stool sample tested negative for C. difficile. Post operatively, patient had increased pressor requirement despite resuscitation efforts. On exam, her ostomy site had a dusky appearance, which prompted an emergent exploratory laparotomy at bedside and resection of an ischemic end ileostomy. Surgical team planned to re-explore abdomen, however her family opted for comfort care and patient expired.
Discussion: Meeting diagnostic criteria for toxic megacolon is not definitive and does not preclude a patient from other etiologies of dilatation. As reflected in this case, large bowel obstructions can present with bowel necrosis and therefore lead to systemic toxicity, presenting in a similar fashion to TM. Identifying a patient’s clinical history and risk factors are critical, such as history of inflammatory bowel disease, clostridium difficile infection, and abdominal surgery. Given this patient’s significant clinical deterioration with worsening sepsis and end organ damage, surgical intervention was indicated regardless of etiology, as there is a high risk of bowel ischemia and perforation in both TM and bowel obstruction.

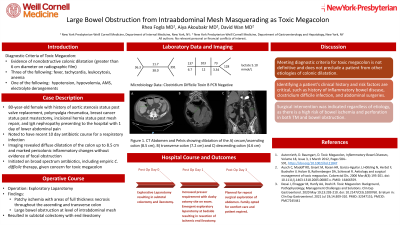
Figure: Figure 1. CT Abdomen and Pelvis showing dilatation of the A) cecum and ascending colon (8.5 cm), B) transverse colon (7.2 cm), and C) descending colon (4.6 cm).
Disclosures:
Rhea Fogla indicated no relevant financial relationships.
Aiya Aboubakr indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Rhea Fogla, MD1, Aiya Aboubakr, MD2, David Wan, BS, MD3. P3062 - Large Bowel Obstruction From Intraabdominal Mesh Masquerading as Toxic Megacolon, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
