Tuesday Poster Session
Category: Practice Management
P4062 - La Bodega: A Co-Localized Approach to Hepatitis C Management Among People Who Use Drugs
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Clive J. Miranda, DO, MS
University at Buffalo
Buffalo, NY
Presenting Author(s)
Clive J. Miranda, DO, MS, Alexander M. Carlson, DO, Slah Khan, MPH, Yousaf Saeed, MD, Naren S. Nallapeta, MBBS, Anthony D. Martinez, MD
University at Buffalo, Buffalo, NY
Introduction: The World Health Organization has targeted the year 2030 for Hepatitis C virus (HCV) elimination. To achieve this, 80% of chronically infected individuals will need to be treated, and new infections will need to be reduced by 90%. The United States is currently not on track to hit this target. New cases of HCV, particularly among people who use drugs (PWUD), are currently outpacing the number of individuals entering into HCV treatment. In order to achieve elimination, treatment uptake among PWUD is essential. We describe our experience at our clinic – La Bodega – which uses an innovative co-localized rapid start, HCV and addition management model to achieve sustained virologic response (SVR) in our patient population.
Methods: A retrospective chart review of our clinic’s database was conducted from 2014 to 2022 for patients treated for HCV. Logistic regression models were used on demographic data to assess statistical significance between variables. Treatment adherence and achievement of SVR among several patient populations were studied.
Results: The La Bodega model creates a partnership with local community substance abuse clinics and provides education on HCV screening and the training of social workers and case managers. A positive HCV antibody test triggers a referral to schedule the patient in our clinic within 7 days. Social workers work closely with patients and provide pre-, during, and post-HCV treatment reminders and education. At the initial visit, patients are provided HCV medications and medically assisted therapy for opiate use disorder from our on-site pharmacy. Our addiction specialists and hepatologists closely monitor and encourage treatment adherence. A total of 1790 patients (66% male) between ages 20-89 being treated for HCV in our clinic were identified. Intention-to-treat (ITT) data was available for 1373 patients (77%). The remaining 417 (23%) did not have data due to loss of follow-up via death, incarceration, or treatment nonadherence. SVR was achieved in 95% of those with ITT data, with no differences in sex, age, or racial populations (p < 0.01). 68 patients with ITT data did not yet achieve SVR but are still actively adhering to follow-up and medication regimens. Those patients who lacked ITT data were more likely to be male (69%) and under 40 (41%).
Discussion: Our clinic’s co-localized model demonstrates high rates of adherence and cure among PWUD with HCV. Further work is needed to improve retention in care, particularly among younger patient populations.

Disclosures:
Clive J. Miranda, DO, MS, Alexander M. Carlson, DO, Slah Khan, MPH, Yousaf Saeed, MD, Naren S. Nallapeta, MBBS, Anthony D. Martinez, MD. P4062 - La Bodega: A Co-Localized Approach to Hepatitis C Management Among People Who Use Drugs, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: The World Health Organization has targeted the year 2030 for Hepatitis C virus (HCV) elimination. To achieve this, 80% of chronically infected individuals will need to be treated, and new infections will need to be reduced by 90%. The United States is currently not on track to hit this target. New cases of HCV, particularly among people who use drugs (PWUD), are currently outpacing the number of individuals entering into HCV treatment. In order to achieve elimination, treatment uptake among PWUD is essential. We describe our experience at our clinic – La Bodega – which uses an innovative co-localized rapid start, HCV and addition management model to achieve sustained virologic response (SVR) in our patient population.
Methods: A retrospective chart review of our clinic’s database was conducted from 2014 to 2022 for patients treated for HCV. Logistic regression models were used on demographic data to assess statistical significance between variables. Treatment adherence and achievement of SVR among several patient populations were studied.
Results: The La Bodega model creates a partnership with local community substance abuse clinics and provides education on HCV screening and the training of social workers and case managers. A positive HCV antibody test triggers a referral to schedule the patient in our clinic within 7 days. Social workers work closely with patients and provide pre-, during, and post-HCV treatment reminders and education. At the initial visit, patients are provided HCV medications and medically assisted therapy for opiate use disorder from our on-site pharmacy. Our addiction specialists and hepatologists closely monitor and encourage treatment adherence. A total of 1790 patients (66% male) between ages 20-89 being treated for HCV in our clinic were identified. Intention-to-treat (ITT) data was available for 1373 patients (77%). The remaining 417 (23%) did not have data due to loss of follow-up via death, incarceration, or treatment nonadherence. SVR was achieved in 95% of those with ITT data, with no differences in sex, age, or racial populations (p < 0.01). 68 patients with ITT data did not yet achieve SVR but are still actively adhering to follow-up and medication regimens. Those patients who lacked ITT data were more likely to be male (69%) and under 40 (41%).
Discussion: Our clinic’s co-localized model demonstrates high rates of adherence and cure among PWUD with HCV. Further work is needed to improve retention in care, particularly among younger patient populations.

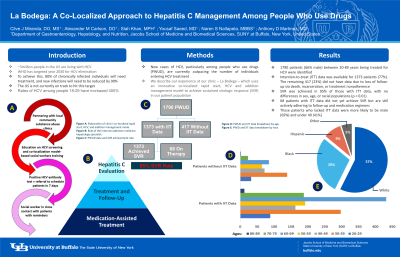
Figure: Figure A: Elaboration of clinic's co-localized rapid start, HCV, and addition management model.
Figure B: Breakdown of our PWUD cohort being treated for HCV, showing a 95% SVR achievement rate.
Figure C: Age breakdown of clinic patients with and without intention-to-treat (ITT) data.
Figure B: Breakdown of our PWUD cohort being treated for HCV, showing a 95% SVR achievement rate.
Figure C: Age breakdown of clinic patients with and without intention-to-treat (ITT) data.
Disclosures:
Clive Miranda indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Slah Khan indicated no relevant financial relationships.
Yousaf Saeed indicated no relevant financial relationships.
Naren Nallapeta indicated no relevant financial relationships.
Anthony Martinez indicated no relevant financial relationships.
Clive J. Miranda, DO, MS, Alexander M. Carlson, DO, Slah Khan, MPH, Yousaf Saeed, MD, Naren S. Nallapeta, MBBS, Anthony D. Martinez, MD. P4062 - La Bodega: A Co-Localized Approach to Hepatitis C Management Among People Who Use Drugs, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
