Tuesday Poster Session
Category: Practice Management
P4069 - A Quality Improvement Analysis of Patient Non-Compliance With Post-ERCP Follow-Up Recommendations in a Predominantly Hispanic Population
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- BT
Bhavi Trivedi, MD
Texas Tech University Health Sciences Center
El Paso, Texas
Presenting Author(s)
Bhavi Trivedi, MD1, Jeff Angelo Taclob, MD1, Brian Lee, DO2, Sukhila Reddy, MD2, Jared Bies, DO2, Melina Ortiz, MD2, Ammar Kalas, MD2, Andrew Ortega, MD2, Marc Zuckerman, MD1, Ricardo Badillo, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Texas Tech, El Paso, TX
Introduction: A timely repeat endoscopic retrograde cholangiopancreatography (ERCP) is necessary for various indications, such as stent removal, to prevent complications. Poor compliance with follow-up can drastically impact outcomes. This quality improvement project aimed to identify underlying reasons for non-compliance by performing a retrospective analysis of patient follow-up after ERCP at our academic tertiary referral center located on the United States/Mexico border among a predominantly Hispanic population.
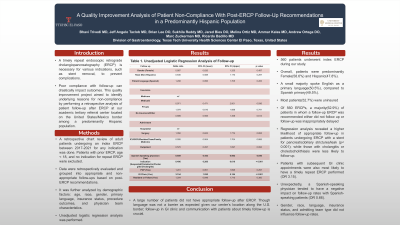
Methods: A retrospective chart review of adult patients undergoing an index ERCP between 2017-2021 for any indication was done. Patients with prior ERCP, age < 18, and no indication for repeat ERCP were excluded. Data were retrospectively evaluated and grouped into appropriate and non-appropriate follow-ups based on post-ERCP recommendations. It was further analyzed by demographic factors: age, race, gender, primary language, insurance status, procedure outcomes, and physician team characteristics. Unadjusted logistic regression analysis was performed.
Results: 560 patients underwent index ERCP during our study. Overall, patients were predominantly Female(58.6%) and Hispanic(47.8%). A small majority spoke English as a primary language(50.5%), compared to Spanish primary(49.5%). Most patients(52.7%) were uninsured(Table 1). Of 560 ERCPs, a majority(62.9%) of patients in whom a follow-up ERCP was recommended either did not follow up or follow-up was inappropriately delayed(Table 2). Regression analysis revealed a higher likelihood of appropriate follow-up in patients undergoing ERCP with a stent for pancreaticobiliary strictures/leak (p< 0.001); while those with cholangitis or choledocholithiasis were less likely to follow up. Patients with subsequent GI clinic appointments were also most likely to have a timely repeat ERCP performed (OR 3.15). Unexpectedly, a Spanish-speaking physician tended to have a negative impact on follow-up rates with Spanish-speaking patients (OR 0.66). Gender, race, language, insurance status, and admitting team type did not influence follow-up rates.
Discussion: A large number of patients did not have appropriate follow-up after ERCP. Though language was not a barrier as expected given our center’s location along the U.S. border; follow-up in GI clinic and communication with patients about timely follow-up is crucial.
Disclosures:
Bhavi Trivedi, MD1, Jeff Angelo Taclob, MD1, Brian Lee, DO2, Sukhila Reddy, MD2, Jared Bies, DO2, Melina Ortiz, MD2, Ammar Kalas, MD2, Andrew Ortega, MD2, Marc Zuckerman, MD1, Ricardo Badillo, MD1. P4069 - A Quality Improvement Analysis of Patient Non-Compliance With Post-ERCP Follow-Up Recommendations in a Predominantly Hispanic Population, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, TX; 2Texas Tech, El Paso, TX
Introduction: A timely repeat endoscopic retrograde cholangiopancreatography (ERCP) is necessary for various indications, such as stent removal, to prevent complications. Poor compliance with follow-up can drastically impact outcomes. This quality improvement project aimed to identify underlying reasons for non-compliance by performing a retrospective analysis of patient follow-up after ERCP at our academic tertiary referral center located on the United States/Mexico border among a predominantly Hispanic population.
Methods: A retrospective chart review of adult patients undergoing an index ERCP between 2017-2021 for any indication was done. Patients with prior ERCP, age < 18, and no indication for repeat ERCP were excluded. Data were retrospectively evaluated and grouped into appropriate and non-appropriate follow-ups based on post-ERCP recommendations. It was further analyzed by demographic factors: age, race, gender, primary language, insurance status, procedure outcomes, and physician team characteristics. Unadjusted logistic regression analysis was performed.
Results: 560 patients underwent index ERCP during our study. Overall, patients were predominantly Female(58.6%) and Hispanic(47.8%). A small majority spoke English as a primary language(50.5%), compared to Spanish primary(49.5%). Most patients(52.7%) were uninsured(Table 1). Of 560 ERCPs, a majority(62.9%) of patients in whom a follow-up ERCP was recommended either did not follow up or follow-up was inappropriately delayed(Table 2). Regression analysis revealed a higher likelihood of appropriate follow-up in patients undergoing ERCP with a stent for pancreaticobiliary strictures/leak (p< 0.001); while those with cholangitis or choledocholithiasis were less likely to follow up. Patients with subsequent GI clinic appointments were also most likely to have a timely repeat ERCP performed (OR 3.15). Unexpectedly, a Spanish-speaking physician tended to have a negative impact on follow-up rates with Spanish-speaking patients (OR 0.66). Gender, race, language, insurance status, and admitting team type did not influence follow-up rates.
Discussion: A large number of patients did not have appropriate follow-up after ERCP. Though language was not a barrier as expected given our center’s location along the U.S. border; follow-up in GI clinic and communication with patients about timely follow-up is crucial.
Disclosures:
Bhavi Trivedi indicated no relevant financial relationships.
Jeff Angelo Taclob indicated no relevant financial relationships.
Brian Lee indicated no relevant financial relationships.
Sukhila Reddy indicated no relevant financial relationships.
Jared Bies indicated no relevant financial relationships.
Melina Ortiz indicated no relevant financial relationships.
Ammar Kalas indicated no relevant financial relationships.
Andrew Ortega indicated no relevant financial relationships.
Marc Zuckerman indicated no relevant financial relationships.
Ricardo Badillo indicated no relevant financial relationships.
Bhavi Trivedi, MD1, Jeff Angelo Taclob, MD1, Brian Lee, DO2, Sukhila Reddy, MD2, Jared Bies, DO2, Melina Ortiz, MD2, Ammar Kalas, MD2, Andrew Ortega, MD2, Marc Zuckerman, MD1, Ricardo Badillo, MD1. P4069 - A Quality Improvement Analysis of Patient Non-Compliance With Post-ERCP Follow-Up Recommendations in a Predominantly Hispanic Population, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
