Tuesday Poster Session
Category: Liver
P3903 - Pyogenic Liver Abscess: A Diagnostic Challenge
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Rohan Tripathi, BS
Saint Louis University
St. Louis, MO
Presenting Author(s)
Rohan Tripathi, BS, Neel Matiwala, BS, Hayden Rotramel, MD, Ryan Plunkett, MD, Ameya deshmukh, DO, Abdallah El Alayli, MD, Maya Mahmoud, MD, Eyad Gharaibeh, MD, Hany Elbeshbeshy, MD
Saint Louis University, St. Louis, MO
Introduction: Entamoeba histolytica is a protozoan parasitic infection spread through fecal-oral transmission. It is commonly found in tropical regions of the globe in areas with poor sanitary conditions and is generally seen in migrants or visitors to endemic areas. Though some literature posits that it can occur in any region of the world, it is very rare in resource-rich nations. This can lead to a delay or error in diagnosis of entamoeba histolytica hepatic abscesses. Here we describe a case of an amebic liver abscess in an immunocompromised patient with IBD.
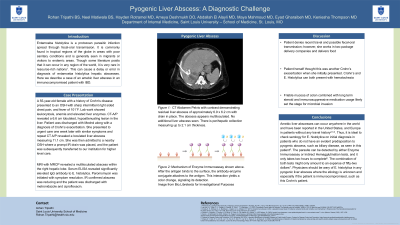
Case Description/Methods: A 55-year-old female with a history of Crohn's disease on azathioprine and adalimumab initially presented to an outside hospital with sharp intermittent right sided chest pain, abdominal pain, and fever to 101 F. Lab work revealed leukocytosis, anemia, elevated liver enzymes and elevated d-dimer. Computed tomography (CT) scan ruled out pulmonary embolism, but revealed a 6.6 cm lobulated, hypoattenuating lesion in the liver. This was attributed to a Crohn’s exacerbation, thus the patient was discharged on a steroid taper. One week later, she presented to urgent care with similar symptoms. Repeat CT imaging revealed a loculated liver abscess measuring 11.1 cm. She was admitted to a nearby hospital for IR-guided abscess drainage followed by laparoscopic evacuation and washout of a congealed and clotted hematoma.
Upon transfer to our institution , she underwent MRCP which showed the multiloculated abscess within the right hepatic lobe and thrombosis of the right hepatic vein. Serum ELISA later revealed a significantly elevated IgG antibody to E. histolytica. Paromycin was initiated and led to symptom resolution. The patient was discharged in stable condition with a course of antibiotics for the infection and apixaban for the hepatic thrombus.
Discussion: Amebic liver abscesses can occur in patients without any travel history and thus, it is reasonable to check serology for E. histolytica in susceptible patient groups. Enzyme immunoassay and indirect hemagglutination tests are relatively inexpensive and can detect the parasite within two hours. Had they been utilized in this patient, they may have prevented the spread of the infection.

Disclosures:
Rohan Tripathi, BS, Neel Matiwala, BS, Hayden Rotramel, MD, Ryan Plunkett, MD, Ameya deshmukh, DO, Abdallah El Alayli, MD, Maya Mahmoud, MD, Eyad Gharaibeh, MD, Hany Elbeshbeshy, MD. P3903 - Pyogenic Liver Abscess: A Diagnostic Challenge, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Saint Louis University, St. Louis, MO
Introduction: Entamoeba histolytica is a protozoan parasitic infection spread through fecal-oral transmission. It is commonly found in tropical regions of the globe in areas with poor sanitary conditions and is generally seen in migrants or visitors to endemic areas. Though some literature posits that it can occur in any region of the world, it is very rare in resource-rich nations. This can lead to a delay or error in diagnosis of entamoeba histolytica hepatic abscesses. Here we describe a case of an amebic liver abscess in an immunocompromised patient with IBD.
Case Description/Methods: A 55-year-old female with a history of Crohn's disease on azathioprine and adalimumab initially presented to an outside hospital with sharp intermittent right sided chest pain, abdominal pain, and fever to 101 F. Lab work revealed leukocytosis, anemia, elevated liver enzymes and elevated d-dimer. Computed tomography (CT) scan ruled out pulmonary embolism, but revealed a 6.6 cm lobulated, hypoattenuating lesion in the liver. This was attributed to a Crohn’s exacerbation, thus the patient was discharged on a steroid taper. One week later, she presented to urgent care with similar symptoms. Repeat CT imaging revealed a loculated liver abscess measuring 11.1 cm. She was admitted to a nearby hospital for IR-guided abscess drainage followed by laparoscopic evacuation and washout of a congealed and clotted hematoma.
Upon transfer to our institution , she underwent MRCP which showed the multiloculated abscess within the right hepatic lobe and thrombosis of the right hepatic vein. Serum ELISA later revealed a significantly elevated IgG antibody to E. histolytica. Paromycin was initiated and led to symptom resolution. The patient was discharged in stable condition with a course of antibiotics for the infection and apixaban for the hepatic thrombus.
Discussion: Amebic liver abscesses can occur in patients without any travel history and thus, it is reasonable to check serology for E. histolytica in susceptible patient groups. Enzyme immunoassay and indirect hemagglutination tests are relatively inexpensive and can detect the parasite within two hours. Had they been utilized in this patient, they may have prevented the spread of the infection.

Figure: Residual multiloculated liver abscess of approximately 6.9 x 6.2 cm with drain in place.
Disclosures:
Rohan Tripathi indicated no relevant financial relationships.
Neel Matiwala indicated no relevant financial relationships.
Hayden Rotramel indicated no relevant financial relationships.
Ryan Plunkett indicated no relevant financial relationships.
Ameya deshmukh indicated no relevant financial relationships.
Abdallah El Alayli indicated no relevant financial relationships.
Maya Mahmoud indicated no relevant financial relationships.
Eyad Gharaibeh indicated no relevant financial relationships.
Hany Elbeshbeshy indicated no relevant financial relationships.
Rohan Tripathi, BS, Neel Matiwala, BS, Hayden Rotramel, MD, Ryan Plunkett, MD, Ameya deshmukh, DO, Abdallah El Alayli, MD, Maya Mahmoud, MD, Eyad Gharaibeh, MD, Hany Elbeshbeshy, MD. P3903 - Pyogenic Liver Abscess: A Diagnostic Challenge, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
