Tuesday Poster Session
Category: Biliary/Pancreas
P2906 - Ampullary Neuroendocrine Tumor "Obstructing" Renal Transplant
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
.jpg)
Murad H. Ali, MD
University at Buffalo
Buffalo, NY
Presenting Author(s)
Murad H. Ali, MD, Clive J. Miranda, DO, MS, Farhan Azad, DO, Elizabeth Z. Gregory, MD, Mayada Ismail, MD, Anoop Prabhu, MD
University at Buffalo, Buffalo, NY
Introduction: Although gastrointestinal (GI) neuroendocrine tumors (NETs) are becoming more frequently diagnosed with increased rates of endoscopy, NETs of the ampulla of Vater are extremely rare.
Case Description/Methods: A 57-year-old male with history of ESRD due to biopsy-proven IgA nephropathy and alcoholic cirrhosis, was admitted to the hospital for renal transplant evaluation. Patient had reported several weeks of melena and fatigue but denied any abdominal pain, jaundice, or weight loss. At admission, hemoglobin 6.8 g/dL and hematocrit 21%. GI was consulted with plan for esophagogastroduodenoscopy (EGD) due to concern for an upper GI bleed. All other labs were unremarkable except for an elevated ALP 227 u/L. CT scan did not reveal any obvious GI lesions.
EGD with push enteroscopy revealed a 3cm and 1cm polypoid masses in the gastric antrum and adjacent to the pylorus, respectively. Further along, a 2x2cm mass was seen in the peri-ampullary area that was oozing a significant amount of blood with multiple arteriovenous malformations in the 2nd and 3rd part of the duodenum. Argon plasma coagulation was performed until hemostasis was achieved. Gastric mass biopsies revealed low-grade epithelial dysplasia, but risk of bleed inhibited duodenal biopsies.
Renal transplant was deferred until diagnosis could be certain and referred to cancer center, where repeat EGD with biopsies and endoscopic ultrasound (EUS) that revealed the gastric antral mass to be a benign, well-differentiated hyperplastic polyp. The previously bleeding ampullary mass grossly appeared as if it had undergone lipomatous changes. EUS showed an enlarged ampulla confined to the papilla with no obvious intraductal involvement. Biopsy revealed positive tumor markers of Cam 5.2, Synaptophysin, Chromogranin A, Ki67 (proliferative index of 1%) indicative of a well-differentiated, low-grade (G1) NET with no mitoses.
Discussion: Ampullary NETs are remarkably rare, with an incidence of < 0.05% of all GI-NETs. With no definitive guidelines, recent literature has suggested that Whipple resection with lymphadenectomy for all ampullary NETs as the most effective therapy due to high-rate metastases. For high-risk patients, endoscopic resection or surgical ampullary resection is an alternative. Our patient’s comorbidities and time sensitivity for transplant, multi-staged stenting of the common bile duct (CBD) with endoscopic mucosal resection of the ampullary NET, and subsequent removal of the CBD stent prior to renal transplant, is planned.

Disclosures:
Murad H. Ali, MD, Clive J. Miranda, DO, MS, Farhan Azad, DO, Elizabeth Z. Gregory, MD, Mayada Ismail, MD, Anoop Prabhu, MD. P2906 - Ampullary Neuroendocrine Tumor "Obstructing" Renal Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Although gastrointestinal (GI) neuroendocrine tumors (NETs) are becoming more frequently diagnosed with increased rates of endoscopy, NETs of the ampulla of Vater are extremely rare.
Case Description/Methods: A 57-year-old male with history of ESRD due to biopsy-proven IgA nephropathy and alcoholic cirrhosis, was admitted to the hospital for renal transplant evaluation. Patient had reported several weeks of melena and fatigue but denied any abdominal pain, jaundice, or weight loss. At admission, hemoglobin 6.8 g/dL and hematocrit 21%. GI was consulted with plan for esophagogastroduodenoscopy (EGD) due to concern for an upper GI bleed. All other labs were unremarkable except for an elevated ALP 227 u/L. CT scan did not reveal any obvious GI lesions.
EGD with push enteroscopy revealed a 3cm and 1cm polypoid masses in the gastric antrum and adjacent to the pylorus, respectively. Further along, a 2x2cm mass was seen in the peri-ampullary area that was oozing a significant amount of blood with multiple arteriovenous malformations in the 2nd and 3rd part of the duodenum. Argon plasma coagulation was performed until hemostasis was achieved. Gastric mass biopsies revealed low-grade epithelial dysplasia, but risk of bleed inhibited duodenal biopsies.
Renal transplant was deferred until diagnosis could be certain and referred to cancer center, where repeat EGD with biopsies and endoscopic ultrasound (EUS) that revealed the gastric antral mass to be a benign, well-differentiated hyperplastic polyp. The previously bleeding ampullary mass grossly appeared as if it had undergone lipomatous changes. EUS showed an enlarged ampulla confined to the papilla with no obvious intraductal involvement. Biopsy revealed positive tumor markers of Cam 5.2, Synaptophysin, Chromogranin A, Ki67 (proliferative index of 1%) indicative of a well-differentiated, low-grade (G1) NET with no mitoses.
Discussion: Ampullary NETs are remarkably rare, with an incidence of < 0.05% of all GI-NETs. With no definitive guidelines, recent literature has suggested that Whipple resection with lymphadenectomy for all ampullary NETs as the most effective therapy due to high-rate metastases. For high-risk patients, endoscopic resection or surgical ampullary resection is an alternative. Our patient’s comorbidities and time sensitivity for transplant, multi-staged stenting of the common bile duct (CBD) with endoscopic mucosal resection of the ampullary NET, and subsequent removal of the CBD stent prior to renal transplant, is planned.

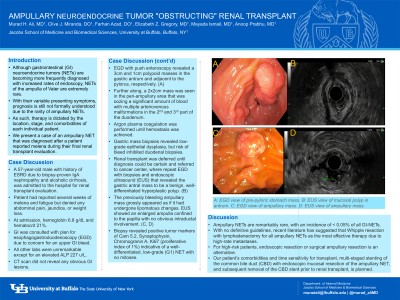
Figure: A: EGD view of pre-pyloric stomach mass.
B: EUS view of mucosal polyp in antrum.
C: EGD view of ampullary mass.
D: EUS view of ampullary mass.
B: EUS view of mucosal polyp in antrum.
C: EGD view of ampullary mass.
D: EUS view of ampullary mass.
Disclosures:
Murad Ali indicated no relevant financial relationships.
Clive Miranda indicated no relevant financial relationships.
Farhan Azad indicated no relevant financial relationships.
Elizabeth Gregory indicated no relevant financial relationships.
Mayada Ismail indicated no relevant financial relationships.
Anoop Prabhu indicated no relevant financial relationships.
Murad H. Ali, MD, Clive J. Miranda, DO, MS, Farhan Azad, DO, Elizabeth Z. Gregory, MD, Mayada Ismail, MD, Anoop Prabhu, MD. P2906 - Ampullary Neuroendocrine Tumor "Obstructing" Renal Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
