Tuesday Poster Session
Category: Biliary/Pancreas
P2909 - A Case of Eosinophilic Cholangiopathy in a Patient With Ulcerative Colitis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Nakia Chung, MD
Stanford University School of Medicine
Redwood City, CA
Presenting Author(s)
Nakia Chung, MD
Stanford University School of Medicine, Redwood City, CA
Introduction: Eosinophilic cholangiopathy (EC) is a rare benign cause of biliary obstruction. No definitive diagnostic criteria for EC exist; however, the following criteria have been suggested: (1) wall thickening/stenosis of the biliary system, (2) histopathologic findings of eosinophilic infiltration, and (3) reversibility of biliary abnormalities with conservative management or following steroid treatment[1]. Many patients with EC require surgery for both diagnostic and therapeutic purposes.
Case Description/Methods: A 55-year-old male with mild ulcerative colitis and acute episcleritis/scleritis (currently on oral steroids) presented with elevated liver tests (AST 111 U/L [Ref Range: 10 – 50 U/L], ALT 211 U/L [Ref Range: 10 – 50 U/L], ALP 242 [Ref Range: 40 – 130 U/L).
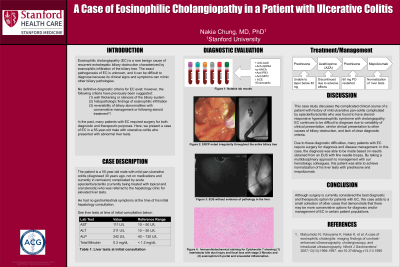
Diagnostic evaluation of elevated liver tests was notable for several different positive auto-immune markers including anti-actin, +anti-dsDNA, +p-ANCA, +anti-PR3, +anti-MPO, and an elevated ACE level. The patient also had hypereosinophilia. A liver biopsy was subsequently performed while the patient was on oral steroids for episcleritis/scleritis, and was notable for chronic perivenular lymphoplasmacytic inflammation with hepatocellular dropout. His liver tests improved when his prednisone dosage was increased; however, they began to increase again when prednisone taper was initiated. Given inability to taper prednisone, azathioprine (AZA) was started. Despite taking prednisone and AZA daily, the patient’s liver tests remained persistently elevated.
Shortly after initiation of the AZA, the patient began to experience persistent nausea, vomiting, and diarrhea prompting him to discontinue all medications. Given his ulcerative colitis, +ANCA, and hypereosinophilia, a vasculitis evaluation was pursued. As part of his vasculitis work-up, MRA abdomen and MRCP was performed and both had findings suggestive of PSC.
He then had an ERCP which was notable for irregularity in the entire biliary tree. An EUS with FNB (performed after patient was off of prednisone for several months) was notable for marked eosinophilic rich infiltrate with bile duct loss consistent with EC. Prednisone was restarted. In consultation with hematology, mepolizumab was started for management of hypereosinophilia. His liver tests eventually normalized.
Discussion: Although surgery is currently considered the best diagnostic and therapeutic option for EC, this case suggests that there are less invasive options available for diagnosis and management of these patients.
Disclosures:
Nakia Chung, MD. P2909 - A Case of Eosinophilic Cholangiopathy in a Patient With Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Stanford University School of Medicine, Redwood City, CA
Introduction: Eosinophilic cholangiopathy (EC) is a rare benign cause of biliary obstruction. No definitive diagnostic criteria for EC exist; however, the following criteria have been suggested: (1) wall thickening/stenosis of the biliary system, (2) histopathologic findings of eosinophilic infiltration, and (3) reversibility of biliary abnormalities with conservative management or following steroid treatment[1]. Many patients with EC require surgery for both diagnostic and therapeutic purposes.
Case Description/Methods: A 55-year-old male with mild ulcerative colitis and acute episcleritis/scleritis (currently on oral steroids) presented with elevated liver tests (AST 111 U/L [Ref Range: 10 – 50 U/L], ALT 211 U/L [Ref Range: 10 – 50 U/L], ALP 242 [Ref Range: 40 – 130 U/L).
Diagnostic evaluation of elevated liver tests was notable for several different positive auto-immune markers including anti-actin, +anti-dsDNA, +p-ANCA, +anti-PR3, +anti-MPO, and an elevated ACE level. The patient also had hypereosinophilia. A liver biopsy was subsequently performed while the patient was on oral steroids for episcleritis/scleritis, and was notable for chronic perivenular lymphoplasmacytic inflammation with hepatocellular dropout. His liver tests improved when his prednisone dosage was increased; however, they began to increase again when prednisone taper was initiated. Given inability to taper prednisone, azathioprine (AZA) was started. Despite taking prednisone and AZA daily, the patient’s liver tests remained persistently elevated.
Shortly after initiation of the AZA, the patient began to experience persistent nausea, vomiting, and diarrhea prompting him to discontinue all medications. Given his ulcerative colitis, +ANCA, and hypereosinophilia, a vasculitis evaluation was pursued. As part of his vasculitis work-up, MRA abdomen and MRCP was performed and both had findings suggestive of PSC.
He then had an ERCP which was notable for irregularity in the entire biliary tree. An EUS with FNB (performed after patient was off of prednisone for several months) was notable for marked eosinophilic rich infiltrate with bile duct loss consistent with EC. Prednisone was restarted. In consultation with hematology, mepolizumab was started for management of hypereosinophilia. His liver tests eventually normalized.
Discussion: Although surgery is currently considered the best diagnostic and therapeutic option for EC, this case suggests that there are less invasive options available for diagnosis and management of these patients.
Disclosures:
Nakia Chung indicated no relevant financial relationships.
Nakia Chung, MD. P2909 - A Case of Eosinophilic Cholangiopathy in a Patient With Ulcerative Colitis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
