Tuesday Poster Session
Category: Liver
P3830 - Venous Thrombosis and Segmental Ischemia in Amebic Liver Abscess: Computed Tomographic Demonstration and its Implications
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Rajeev N. Priyadarshi, MD
All India Institute of Medical Sciences
Patna, Bihar, India
Presenting Author(s)
Rajeev N. Priyadarshi, MD1, Lisna Sherin, MD2, Ramesh Kumar, MBBS, MD, DM1
1All India Institute of Medical Sciences, Patna, Bihar, India; 2All India Institute of Medical Sciences, New Delhi, Delhi, India
Introduction: Ischemia caused by venous thrombosis has been implicated in the pathogenesis of amebic liver abscess (ALA). This study aimed to report venous thrombosis and associated perfusion defect indicating segmental ischemia in ALA using multidetector computed tomography (MDCT).
Methods: MDCT images of 62 patients with ALA were reviewed for venous thrombosis and associated perfusion abnormalities. Hypoperfusion was considered when segmental or subsegmental hypoenhancement (attenuation value < 30HU compared to the healthy parenchyma) was detected surrounding the ALA on the venous phase of CT examination. Response to medical therapy and the outcomes were assessed in the patients with venous thrombosis.
Results: The study found 43 (69%) patients with venous thrombosis: portal vein thrombosis (PVT) occurred in 39, hepatic vein thrombosis (HVT) in 37 and inferior vena cava (IVC) thrombosis in 4. Combined PVT and HVT occurred in 33 (77%) patients. The portal vein thrombi remained localized in subsegmental branches in 25 patients and extended to segmental branches in 14. The hepatic vein thrombi were confined to peripheral branches in 18 patients; they progressed to the main trunk in 19 and to the IVC in 4. A wedge-shaped hypoattenuating zone suggesting ischemia was identified in 33 (77%) patients in portal phase: 31 had combined PVT and HVT, 2 had HVT alone, but none had PVT alone. It occurred significantly more often with combined PVT and HVT than HVT alone (p = 0.05). Laboratory data revealed marked leukocytosis (average total leukocyte counts 29,882 ± 9,243 /μL) in all patients. The average level of alanine aminotransferase was 206.3 ± 133.6 U/L, of aspartate aminotransferase was 233.6 ± 122.4 U/L, of alkaline phosphatase was 408.1 ± 188.1 U/L, and of total bilirubin was 2.9 ± 2.1 mg/dL. All patients were symptomatic despite medical therapy and therefore required percutaneous drainage. About half of the patients were identified with ruptured abscesses. 13 patients had thickened cecal wall indicating amebic colitis and one had ruptured appendix due to amebic appendicitis. Segmental atrophy of the liver was observed in seven of nine patients who underwent follow-up CT.
Discussion: Combined PVT and HVT commonly occur with ALA and often manifests as segmental hypoperfusion in portal venous phase, indicating segmental ischemia. The detection of such events by CT may be indicative of severe disease that requires aggressive management involving percutaneous drainage.

Disclosures:
Rajeev N. Priyadarshi, MD1, Lisna Sherin, MD2, Ramesh Kumar, MBBS, MD, DM1. P3830 - Venous Thrombosis and Segmental Ischemia in Amebic Liver Abscess: Computed Tomographic Demonstration and its Implications, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1All India Institute of Medical Sciences, Patna, Bihar, India; 2All India Institute of Medical Sciences, New Delhi, Delhi, India
Introduction: Ischemia caused by venous thrombosis has been implicated in the pathogenesis of amebic liver abscess (ALA). This study aimed to report venous thrombosis and associated perfusion defect indicating segmental ischemia in ALA using multidetector computed tomography (MDCT).
Methods: MDCT images of 62 patients with ALA were reviewed for venous thrombosis and associated perfusion abnormalities. Hypoperfusion was considered when segmental or subsegmental hypoenhancement (attenuation value < 30HU compared to the healthy parenchyma) was detected surrounding the ALA on the venous phase of CT examination. Response to medical therapy and the outcomes were assessed in the patients with venous thrombosis.
Results: The study found 43 (69%) patients with venous thrombosis: portal vein thrombosis (PVT) occurred in 39, hepatic vein thrombosis (HVT) in 37 and inferior vena cava (IVC) thrombosis in 4. Combined PVT and HVT occurred in 33 (77%) patients. The portal vein thrombi remained localized in subsegmental branches in 25 patients and extended to segmental branches in 14. The hepatic vein thrombi were confined to peripheral branches in 18 patients; they progressed to the main trunk in 19 and to the IVC in 4. A wedge-shaped hypoattenuating zone suggesting ischemia was identified in 33 (77%) patients in portal phase: 31 had combined PVT and HVT, 2 had HVT alone, but none had PVT alone. It occurred significantly more often with combined PVT and HVT than HVT alone (p = 0.05). Laboratory data revealed marked leukocytosis (average total leukocyte counts 29,882 ± 9,243 /μL) in all patients. The average level of alanine aminotransferase was 206.3 ± 133.6 U/L, of aspartate aminotransferase was 233.6 ± 122.4 U/L, of alkaline phosphatase was 408.1 ± 188.1 U/L, and of total bilirubin was 2.9 ± 2.1 mg/dL. All patients were symptomatic despite medical therapy and therefore required percutaneous drainage. About half of the patients were identified with ruptured abscesses. 13 patients had thickened cecal wall indicating amebic colitis and one had ruptured appendix due to amebic appendicitis. Segmental atrophy of the liver was observed in seven of nine patients who underwent follow-up CT.
Discussion: Combined PVT and HVT commonly occur with ALA and often manifests as segmental hypoperfusion in portal venous phase, indicating segmental ischemia. The detection of such events by CT may be indicative of severe disease that requires aggressive management involving percutaneous drainage.

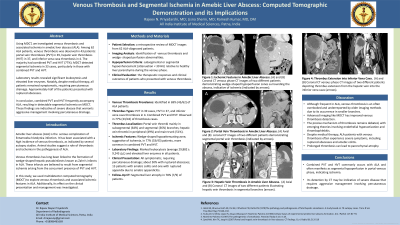
Figure: Coronal contrast enhanced CT images of three different patients with amebic liver abscesses demonstrating thrombosed hepatic veins (arrowheads in Panel A and B) or portal vein (arrow in Panel C). Note the presence of a large wedge-shaped hypoattenuating zone (asterisk) surrounding the abscesses indicating segmental hypoperfusion in all cases.
Disclosures:
Rajeev Priyadarshi indicated no relevant financial relationships.
Lisna Sherin indicated no relevant financial relationships.
Ramesh Kumar indicated no relevant financial relationships.
Rajeev N. Priyadarshi, MD1, Lisna Sherin, MD2, Ramesh Kumar, MBBS, MD, DM1. P3830 - Venous Thrombosis and Segmental Ischemia in Amebic Liver Abscess: Computed Tomographic Demonstration and its Implications, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
