Tuesday Poster Session
Category: Liver
P3831 - Timing of Paracentesis in Relation to Antibiotic Therapy in Cirrhotic Patients with SBP: A Quality Improvement Project
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Mena Tawfik, MD
Parkview Medical Center
Pueblo, CO
Presenting Author(s)
Mena Tawfik, MD, Ramy Sekla, MD, Uday Patel, DO, Aleena Sammar, MD, Lindsey Longfellow, DO, Christopher Calcagno, DO
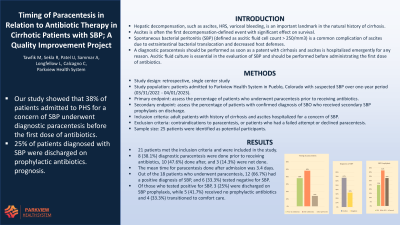
Parkview Medical Center, Pueblo, CO
Introduction: Hepatic decompensation, such as ascites, HRS, variceal bleeding, is an important landmark in the natural history of cirrhosis. Ascites is often the first decompensation-defined event with significant effect on survival. Spontaneous bacterial peritonitis (SBP) is a common complication of ascites due to extraintestinal bacterial translocation and decreased host defenses. Diagnosis of SBP is defined as ascitic fluid cell count > 250/mm3. A diagnostic paracentesis should be performed as soon as a patent with cirrhosis and ascites is hospitalized emergently for any reason. Ascitic fluid culture is essential in the evaluation of SBP and should be performed before administrating the first dose of antibiotics.
Methods: We conducted a retrospective, single center study including patients admitted to Parkview Health System in Pueblo, Colorado with suspected SBP over one-year period (03/31/2022 - 04/01/2023). The primary endpoint was to assess the percentage of patients who underwent paracentesis prior to receiving antibiotics. A secondary endpoint was to assess the percentage of patients who received secondary SBP prophylaxis on discharge. All adult patients with history of cirrhosis and ascites hospitalized for a concern of SBP were included. Exclusion criteria were contraindications to paracentesis, or patients who had a failed attempt or declined paracentesis. A total of 25 patients were identified as potential participants.
Results: 21 patients met the inclusion criteria and were included in the study. Out of those patients, 8 (38.1%) diagnostic paracentesis were done prior to receiving antibiotics, 10 (47.6%) done after, and 3 (14.3%) were not done. The mean time for paracentesis done after admission was 3.4 days. Out of the 18 patients who underwent paracentesis, 12 (66.7%) had a positive diagnosis of SBP, and 6 (33.3%) tested negative for SBP. Of those who tested positive for SBP, 3 (25%) were discharged on SBP prophylaxis, while 5 (41.7%) received no prophylactic antibiotics and 4 (33.3%) transitioned to comfort care.
Discussion: Our project aimed to improve adherence to current recommendations as this may affect immediate patient care and eventually overall prognosis. Many efforts were made in this regards such as multiple educational conferences. We also created an EMR order set for ascitic fluid analysis to facilitate ordering for providers. Our goal is to increase the percentage to more than 60% in the next 6 months.
Disclosures:
Mena Tawfik, MD, Ramy Sekla, MD, Uday Patel, DO, Aleena Sammar, MD, Lindsey Longfellow, DO, Christopher Calcagno, DO. P3831 - Timing of Paracentesis in Relation to Antibiotic Therapy in Cirrhotic Patients with SBP: A Quality Improvement Project, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Parkview Medical Center, Pueblo, CO
Introduction: Hepatic decompensation, such as ascites, HRS, variceal bleeding, is an important landmark in the natural history of cirrhosis. Ascites is often the first decompensation-defined event with significant effect on survival. Spontaneous bacterial peritonitis (SBP) is a common complication of ascites due to extraintestinal bacterial translocation and decreased host defenses. Diagnosis of SBP is defined as ascitic fluid cell count > 250/mm3. A diagnostic paracentesis should be performed as soon as a patent with cirrhosis and ascites is hospitalized emergently for any reason. Ascitic fluid culture is essential in the evaluation of SBP and should be performed before administrating the first dose of antibiotics.
Methods: We conducted a retrospective, single center study including patients admitted to Parkview Health System in Pueblo, Colorado with suspected SBP over one-year period (03/31/2022 - 04/01/2023). The primary endpoint was to assess the percentage of patients who underwent paracentesis prior to receiving antibiotics. A secondary endpoint was to assess the percentage of patients who received secondary SBP prophylaxis on discharge. All adult patients with history of cirrhosis and ascites hospitalized for a concern of SBP were included. Exclusion criteria were contraindications to paracentesis, or patients who had a failed attempt or declined paracentesis. A total of 25 patients were identified as potential participants.
Results: 21 patients met the inclusion criteria and were included in the study. Out of those patients, 8 (38.1%) diagnostic paracentesis were done prior to receiving antibiotics, 10 (47.6%) done after, and 3 (14.3%) were not done. The mean time for paracentesis done after admission was 3.4 days. Out of the 18 patients who underwent paracentesis, 12 (66.7%) had a positive diagnosis of SBP, and 6 (33.3%) tested negative for SBP. Of those who tested positive for SBP, 3 (25%) were discharged on SBP prophylaxis, while 5 (41.7%) received no prophylactic antibiotics and 4 (33.3%) transitioned to comfort care.
Discussion: Our project aimed to improve adherence to current recommendations as this may affect immediate patient care and eventually overall prognosis. Many efforts were made in this regards such as multiple educational conferences. We also created an EMR order set for ascitic fluid analysis to facilitate ordering for providers. Our goal is to increase the percentage to more than 60% in the next 6 months.
Disclosures:
Mena Tawfik indicated no relevant financial relationships.
Ramy Sekla indicated no relevant financial relationships.
Uday Patel indicated no relevant financial relationships.
Aleena Sammar indicated no relevant financial relationships.
Lindsey Longfellow indicated no relevant financial relationships.
Christopher Calcagno indicated no relevant financial relationships.
Mena Tawfik, MD, Ramy Sekla, MD, Uday Patel, DO, Aleena Sammar, MD, Lindsey Longfellow, DO, Christopher Calcagno, DO. P3831 - Timing of Paracentesis in Relation to Antibiotic Therapy in Cirrhotic Patients with SBP: A Quality Improvement Project, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
