Tuesday Poster Session
Category: Liver
P3837 - Understanding Clinical Outcomes Associated With Mycophenolate Use Among Liver and Renal Transplant Recipients Infected With SARS-CoV2
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- AF
Ashley Francis, BS
Wayne State University School of Medicine
Detroit, Michigan
Presenting Author(s)
Ashley Francis, BS1, Sara Farooqui, BS1, Suraj Suresh, MD2, Syed-Mohammed Jafri, MD3
1Wayne State University School of Medicine, Detroit, MI; 2Henry Ford Hospital, Detroit, MI; 3Henry Ford Health System, Detroit, MI
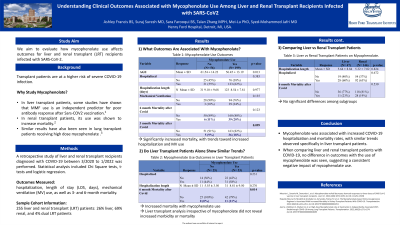
Introduction: The use of long-term immunosuppressants in solid organ transplant recipients has been shown to increase COVID-19 related morbidity and mortality. However, further studies examining outcomes for specific types of immunosuppressants is limited. We aim to evaluate how mycophenolate use affects outcomes for liver and renal transplant (LRT) recipients infected with SARS-CoV-2.
Methods: A retrospective study of LRT recipients diagnosed with COVID-19 between 3/2020 to 1/2022 was performed. We recorded data on patient demographics, immunosuppressants, vaccine dose numbers, MAB treatment, hospitalization, length of stay (LOS, days), mechanical ventilation (MV) use, as well as 3- and 6-month mortality. Statistical analysis included Chi Square tests, t-tests and logistic regression.
Results: Out of 255 LRT recipients diagnosed with COVID-19, 68 (26%) were liver transplant patients, 177 (69%) were renal transplant patients, and 10 (4%) had received dual LRT. Comparing liver and renal transplant patients, there were no significant differences in hospitalization and mortality rates. This analysis was further stratified to examine the effects of Mycophenolate. Among 199 patients using mycophenolate, there was a higher incidence of hospitalization (62% vs. 55% p =0.383), mechanical ventilation (24% vs. 10% p=0.135), and mortality at 3 and 6 months compared to non-users (18% vs. 9% p=0.099 and 20% vs. 11% p=0.123). In the liver transplant subgroup (78 patients, 68% on mycophenolate), mycophenolate use was associated with increased hospitalization rates (58% vs. 44% p=0.231) and higher mortality at 3 and 6 months compared to non-users (19% vs. 0% p=0.020 and 11% vs. 0% p=0.014, respectively). In the renal transplant subgroup (187 patients, 81% on mycophenolate), there was no difference in hospitalization rates between users and non-users (62% vs. 62%). When comparing 47 liver to 146 renal transplant patients on mycophenolate (excluding dual LRT patients), there were no significant differences in hospitalization (p=0.672), mortality at 3 months (p=0.595), or mortality at 6 months (p=0.530).
Discussion: Our data demonstrates that mycophenolate was associated with increased hospitalization and mortality rates, with similar trends observed specifically in liver transplant patients. Furthermore, there was no difference in outcomes with the use of mycophenolate when comparing liver and renal transplant patients, indicating consistent trends of mycophenolate impacting morbidity.
Disclosures:
Ashley Francis, BS1, Sara Farooqui, BS1, Suraj Suresh, MD2, Syed-Mohammed Jafri, MD3. P3837 - Understanding Clinical Outcomes Associated With Mycophenolate Use Among Liver and Renal Transplant Recipients Infected With SARS-CoV2, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Wayne State University School of Medicine, Detroit, MI; 2Henry Ford Hospital, Detroit, MI; 3Henry Ford Health System, Detroit, MI
Introduction: The use of long-term immunosuppressants in solid organ transplant recipients has been shown to increase COVID-19 related morbidity and mortality. However, further studies examining outcomes for specific types of immunosuppressants is limited. We aim to evaluate how mycophenolate use affects outcomes for liver and renal transplant (LRT) recipients infected with SARS-CoV-2.
Methods: A retrospective study of LRT recipients diagnosed with COVID-19 between 3/2020 to 1/2022 was performed. We recorded data on patient demographics, immunosuppressants, vaccine dose numbers, MAB treatment, hospitalization, length of stay (LOS, days), mechanical ventilation (MV) use, as well as 3- and 6-month mortality. Statistical analysis included Chi Square tests, t-tests and logistic regression.
Results: Out of 255 LRT recipients diagnosed with COVID-19, 68 (26%) were liver transplant patients, 177 (69%) were renal transplant patients, and 10 (4%) had received dual LRT. Comparing liver and renal transplant patients, there were no significant differences in hospitalization and mortality rates. This analysis was further stratified to examine the effects of Mycophenolate. Among 199 patients using mycophenolate, there was a higher incidence of hospitalization (62% vs. 55% p =0.383), mechanical ventilation (24% vs. 10% p=0.135), and mortality at 3 and 6 months compared to non-users (18% vs. 9% p=0.099 and 20% vs. 11% p=0.123). In the liver transplant subgroup (78 patients, 68% on mycophenolate), mycophenolate use was associated with increased hospitalization rates (58% vs. 44% p=0.231) and higher mortality at 3 and 6 months compared to non-users (19% vs. 0% p=0.020 and 11% vs. 0% p=0.014, respectively). In the renal transplant subgroup (187 patients, 81% on mycophenolate), there was no difference in hospitalization rates between users and non-users (62% vs. 62%). When comparing 47 liver to 146 renal transplant patients on mycophenolate (excluding dual LRT patients), there were no significant differences in hospitalization (p=0.672), mortality at 3 months (p=0.595), or mortality at 6 months (p=0.530).
Discussion: Our data demonstrates that mycophenolate was associated with increased hospitalization and mortality rates, with similar trends observed specifically in liver transplant patients. Furthermore, there was no difference in outcomes with the use of mycophenolate when comparing liver and renal transplant patients, indicating consistent trends of mycophenolate impacting morbidity.
Disclosures:
Ashley Francis indicated no relevant financial relationships.
Sara Farooqui indicated no relevant financial relationships.
Suraj Suresh indicated no relevant financial relationships.
Syed-Mohammed Jafri: Gilead, Takeda, Abbvie – Advisor or Review Panel Member, Speakers Bureau.
Ashley Francis, BS1, Sara Farooqui, BS1, Suraj Suresh, MD2, Syed-Mohammed Jafri, MD3. P3837 - Understanding Clinical Outcomes Associated With Mycophenolate Use Among Liver and Renal Transplant Recipients Infected With SARS-CoV2, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
