Tuesday Poster Session
Category: IBD
P3615 - Assessment of Mucosal Healing in a Predominantly African American General Gastroenterology Clinic
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Angy Hanna, MD
Detroit Medical Center
Detroit, MI
Presenting Author(s)
Angy Hanna, MD1, Paul Kim, BA2, Jing Wang, MD3, Jasdeep Bathla, DO4, Bashar Mohamad, MD5, Paul H. Naylor, PhD6, Milton G. Mutchnick, MD2
1Detroit Medical Center, Detroit, MI; 2Wayne State University School of Medicine, Detroit, MI; 3Detroit Medical Center/Wayne State University, Detroit, MI; 4Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 5Wayne State University, Detroit, MI; 6Wayne State University School of Medicine, Hazel Park, MI
Introduction: Many patients with Crohn’s Disease (CD) are treated in general gastroenterology (GI) practices as opposed to dedicated IBD clinics. Most of the current literature is from IBD specialty physicians, so real world data is valuable to demonstrate care given by general GI physicians.
Methods: Using the ICD-10 code for CD and medical record review, 136 patients with at least 1 GI evaluation were identified. Endoscopic evaluation at earliest visit was scored by a single GI fellow as either Mild (minimal inflammation) Moderate (modest inflammation, bleeding, or ulcerations) or Severe (significant inflammation and multiple ulcerations, bleeding, or fistula complications). Endoscopic change over time with respect to current therapy was scored as improved, stable, or not heling (worsening) as compared to the initial staging.
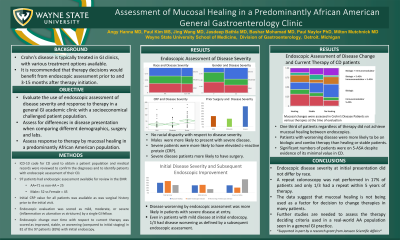
Results: Of the 136 CD patients, 92 (72%) had an endoscopic assessment available for review at their early Gi visits and 78 had a repeat endoscopy. There were no differences in disease severity with respect to race, but males were more likely to have severe disease (Table1). Severe disease patients were also more likely to have had surgery and elevated C-reactive Protein (CRP). Repeat endoscopies had an average time of 7 years apart and only 23 (30%) were within 5 years. Patients with the most severe disease at early visit were more likely to have a worsening of disease on therapy (54%) as compared to mild (31%) and moderate (15%) (Table 1). With respect to therapy and endoscopic improvement, patients with worsening disease were more likely to be on biologic and combination therapy than healing or stable patients (Figure 1).
Discussion: Endoscopic disease severity for CD at the earliest visit was not different with respect to race. Severity of disease was reflected in both surgery and inflammation as defined by CRP. Severity was also reflected in the types of therapy with biologics and combination of biologics and immunomodulators being more likely as compared to mild and moderate patients. The fact that only 30% of patients had a repeat endoscopy within 5 years suggests that mucosal healing may not be used in many patients in general Gi practices. Further studies to address the issue of current therapy, disease site and the use of mucosal healing assessment are needed.

Disclosures:
Angy Hanna, MD1, Paul Kim, BA2, Jing Wang, MD3, Jasdeep Bathla, DO4, Bashar Mohamad, MD5, Paul H. Naylor, PhD6, Milton G. Mutchnick, MD2. P3615 - Assessment of Mucosal Healing in a Predominantly African American General Gastroenterology Clinic, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Detroit Medical Center, Detroit, MI; 2Wayne State University School of Medicine, Detroit, MI; 3Detroit Medical Center/Wayne State University, Detroit, MI; 4Wayne State University School of Medicine / Detroit Medical Center, Detroit, MI; 5Wayne State University, Detroit, MI; 6Wayne State University School of Medicine, Hazel Park, MI
Introduction: Many patients with Crohn’s Disease (CD) are treated in general gastroenterology (GI) practices as opposed to dedicated IBD clinics. Most of the current literature is from IBD specialty physicians, so real world data is valuable to demonstrate care given by general GI physicians.
Methods: Using the ICD-10 code for CD and medical record review, 136 patients with at least 1 GI evaluation were identified. Endoscopic evaluation at earliest visit was scored by a single GI fellow as either Mild (minimal inflammation) Moderate (modest inflammation, bleeding, or ulcerations) or Severe (significant inflammation and multiple ulcerations, bleeding, or fistula complications). Endoscopic change over time with respect to current therapy was scored as improved, stable, or not heling (worsening) as compared to the initial staging.
Results: Of the 136 CD patients, 92 (72%) had an endoscopic assessment available for review at their early Gi visits and 78 had a repeat endoscopy. There were no differences in disease severity with respect to race, but males were more likely to have severe disease (Table1). Severe disease patients were also more likely to have had surgery and elevated C-reactive Protein (CRP). Repeat endoscopies had an average time of 7 years apart and only 23 (30%) were within 5 years. Patients with the most severe disease at early visit were more likely to have a worsening of disease on therapy (54%) as compared to mild (31%) and moderate (15%) (Table 1). With respect to therapy and endoscopic improvement, patients with worsening disease were more likely to be on biologic and combination therapy than healing or stable patients (Figure 1).
Discussion: Endoscopic disease severity for CD at the earliest visit was not different with respect to race. Severity of disease was reflected in both surgery and inflammation as defined by CRP. Severity was also reflected in the types of therapy with biologics and combination of biologics and immunomodulators being more likely as compared to mild and moderate patients. The fact that only 30% of patients had a repeat endoscopy within 5 years suggests that mucosal healing may not be used in many patients in general Gi practices. Further studies to address the issue of current therapy, disease site and the use of mucosal healing assessment are needed.

Figure: Figure 1 Mucosal Healing and Current Therapy. Mucosal healing as assessed by early vs recent endoscopic reports was compared to the therapy which was in current use. The width of the bars represent the size of the population and the height represent the proportion of each therapy. Patients with worsening healing were less likely to be on single therapy and more likely to be on a biological agent.
Disclosures:
Angy Hanna indicated no relevant financial relationships.
Paul Kim indicated no relevant financial relationships.
Jing Wang indicated no relevant financial relationships.
Jasdeep Bathla indicated no relevant financial relationships.
Bashar Mohamad indicated no relevant financial relationships.
Paul Naylor: Janssen Biotech Inc – Grant/Research Support.
Milton Mutchnick: Chronic Liver Disease Foundation – Speakers Bureau. Janssen Biotech Inc – Grant/Research Support.
Angy Hanna, MD1, Paul Kim, BA2, Jing Wang, MD3, Jasdeep Bathla, DO4, Bashar Mohamad, MD5, Paul H. Naylor, PhD6, Milton G. Mutchnick, MD2. P3615 - Assessment of Mucosal Healing in a Predominantly African American General Gastroenterology Clinic, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
