Tuesday Poster Session
Category: IBD
P3619 - Gender-Specific Outcomes and Complications in Patients With Inflammatory Bowel Disease Hospitalized for COVID-19: A National Analysis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Christian Karime, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Christian Karime, MD1, Miguel Salazar, MD2, Cecily Black, RN1, Muhammad B. Hammami, MD2, Jana G.. Hashash, MD, MSc, FACG1, Francis A. Farraye, MD, MSc, MACG1
1Mayo Clinic, Jacksonville, FL; 2University of California Riverside, Riverside, CA
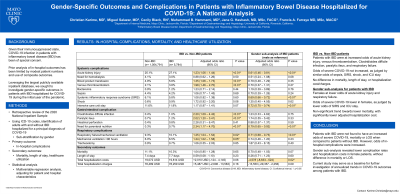
Introduction: With both disease-mediated and treatment-derived immunosuppression, gender-specific outcomes in patients with inflammatory bowel disease (IBD) hospitalized for COVID-19 remains unknown.
Methods: We performed a retrospective review of the 2020 National Inpatient Sample (NIS) ICD10-CM and PCS codes for patients admitted with a principal diagnosis of COVID-19. Patients were subdivided into those with or without IBD, with gender-based subanalysis. Primary outcomes were in-hospital complications. Secondary outcomes were mortality, length of stay (LOS), and healthcare utilization. Frequencies and demographics were compared between groups. Multivariate regression analysis was performed to adjust for patient and hospital characteristics.
Results: We identified a total of 1,060,575 discharges with a principal diagnosis of COVID-19, of which 5,784 were in patients with IBD. Patients with IBD admitted for COVID-19 were more likely to be female (53.5% vs 47.1%, p< 0.01) and White (73.9% vs 50.8%, p< 0.01). Adjusting for patient characteristics on multivariate regression, patients with IBD admitted for COVID-19 had higher odds of developing paralytic ileus (aOR 2.02, p< 0.01), venous thromboembolism (aOR 1.98, p< 0.01), clostridioides difficile infection (aOR 2.20, p< 0.01), acute kidney injury (AKI; aOR 1.23, p< 0.01), and need for blood products (aOR 1.35, p< 0.01). Despite lower odds of acute respiratory failure (ARF; aOR 0.79, p< 0.01), higher odds of endotracheal intubation (aOR 1.25, p=0.02) and mechanical ventilation > 96 hours (aOR 1.24, p=0.05) was noted. On gender-based subanalysis, females with IBD had lower odds of ARF (aOR 0.72, p< 0.01), endotracheal intubation (aOR 0.54, p< 0.01) and AKI (aOR 0.61, p< 0.01) than males. For secondary outcomes, no difference in mortality, LOS, hospitalization costs or charges was noted for patients with vs without IBD. Gender-based subanalysis in patients with IBD revealed decreased hospitalization costs (-$4,578 per admission, p=0.02) and a non-significant trend towards lower mortality in females (aOR 0.70, p=0.07).
Discussion: In the current 2020 national analysis of COVID-19 hospitalizations, patients with IBD were not found to have an increased mortality or LOS. However, in-hospital complications were found to be more frequent. Gender-based subanalysis revealed lower complication rates and hospitalization costs in females, but no difference in mortality or LOS. Further studies are needed to evaluate trends from 2021-2022 NIS data when available.
Disclosures:
Christian Karime, MD1, Miguel Salazar, MD2, Cecily Black, RN1, Muhammad B. Hammami, MD2, Jana G.. Hashash, MD, MSc, FACG1, Francis A. Farraye, MD, MSc, MACG1. P3619 - Gender-Specific Outcomes and Complications in Patients With Inflammatory Bowel Disease Hospitalized for COVID-19: A National Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Mayo Clinic, Jacksonville, FL; 2University of California Riverside, Riverside, CA
Introduction: With both disease-mediated and treatment-derived immunosuppression, gender-specific outcomes in patients with inflammatory bowel disease (IBD) hospitalized for COVID-19 remains unknown.
Methods: We performed a retrospective review of the 2020 National Inpatient Sample (NIS) ICD10-CM and PCS codes for patients admitted with a principal diagnosis of COVID-19. Patients were subdivided into those with or without IBD, with gender-based subanalysis. Primary outcomes were in-hospital complications. Secondary outcomes were mortality, length of stay (LOS), and healthcare utilization. Frequencies and demographics were compared between groups. Multivariate regression analysis was performed to adjust for patient and hospital characteristics.
Results: We identified a total of 1,060,575 discharges with a principal diagnosis of COVID-19, of which 5,784 were in patients with IBD. Patients with IBD admitted for COVID-19 were more likely to be female (53.5% vs 47.1%, p< 0.01) and White (73.9% vs 50.8%, p< 0.01). Adjusting for patient characteristics on multivariate regression, patients with IBD admitted for COVID-19 had higher odds of developing paralytic ileus (aOR 2.02, p< 0.01), venous thromboembolism (aOR 1.98, p< 0.01), clostridioides difficile infection (aOR 2.20, p< 0.01), acute kidney injury (AKI; aOR 1.23, p< 0.01), and need for blood products (aOR 1.35, p< 0.01). Despite lower odds of acute respiratory failure (ARF; aOR 0.79, p< 0.01), higher odds of endotracheal intubation (aOR 1.25, p=0.02) and mechanical ventilation > 96 hours (aOR 1.24, p=0.05) was noted. On gender-based subanalysis, females with IBD had lower odds of ARF (aOR 0.72, p< 0.01), endotracheal intubation (aOR 0.54, p< 0.01) and AKI (aOR 0.61, p< 0.01) than males. For secondary outcomes, no difference in mortality, LOS, hospitalization costs or charges was noted for patients with vs without IBD. Gender-based subanalysis in patients with IBD revealed decreased hospitalization costs (-$4,578 per admission, p=0.02) and a non-significant trend towards lower mortality in females (aOR 0.70, p=0.07).
Discussion: In the current 2020 national analysis of COVID-19 hospitalizations, patients with IBD were not found to have an increased mortality or LOS. However, in-hospital complications were found to be more frequent. Gender-based subanalysis revealed lower complication rates and hospitalization costs in females, but no difference in mortality or LOS. Further studies are needed to evaluate trends from 2021-2022 NIS data when available.
Disclosures:
Christian Karime indicated no relevant financial relationships.
Miguel Salazar indicated no relevant financial relationships.
Cecily Black indicated no relevant financial relationships.
Muhammad Hammami indicated no relevant financial relationships.
Jana Hashash: Iterative Health – Grant/Research Support.
Francis Farraye: AbbVie – Advisory Committee/Board Member. Avalo Therapeutics – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. GSK – Advisory Committee/Board Member. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member. Janssen – Advisory Committee/Board Member. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz Immunology – Advisory Committee/Board Member. Sebela – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Christian Karime, MD1, Miguel Salazar, MD2, Cecily Black, RN1, Muhammad B. Hammami, MD2, Jana G.. Hashash, MD, MSc, FACG1, Francis A. Farraye, MD, MSc, MACG1. P3619 - Gender-Specific Outcomes and Complications in Patients With Inflammatory Bowel Disease Hospitalized for COVID-19: A National Analysis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.

