Tuesday Poster Session
Category: IBD
P3624 - Intestinal Microbiota Transplant vs Standard Management in Patients With Inflammatory Bowel Disease: Systematic Review and Meta-Analysis of Randomized Controlled Trials
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall

Ifrah Fatima, MD
University of Missouri-Kansas City
Kansas City, MO
Presenting Author(s)
Ifrah Fatima, MD1, Jagadish Koyi, MD1, Ben Ponvilawan, MD2, Vineel Mallavarapu, 3, Babu Mohan, MD, MS4
1University of Missouri-Kansas City, Kansas City, MO; 2UMKC School of Medicine, Kansas City, MO; 3Carver College of Medicine, University of Iowa, Iowa City, IA; 4University of Utah Health School of Medicine, Salt Lake City, UT
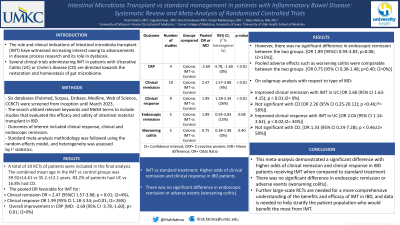
Introduction: The role and clinical indications of Intestinal microbiota transplant (IMT) have witnessed increasing interest owing to advancements in disease process research and its role in dysbiosis. Several clinical trials administering IMT in patients with Ulcerative Colitis (UC) or Crohn's disease (CD) are directed towards the restoration and homeostasis of gut microbiome.
Methods: Six databases (Pubmed, Scopus, Embase, Medline, Web of Science, CCRCT) were screened from inception until March 2023. The search utilized relevant keywords and MeSH terms to include studies that evaluated the efficacy and safety of intestinal material transplant in IBD. Outcomes of interest included clinical response, clinical and endoscopic remission.
Standard meta-analysis methodology was followed using the random-effects model, and heterogeneity was assessed by I2 statistics.
Results: A total of 10 RCTs of patients were included in the final analysis. The combined mean age in the IMT vs control groups was 39.92±14.61 vs 35.2.±12.1 years. 83.2% of patients had UC vs 16.8% had CD.
The pooled OR for clinical remission was favorable with IMT, OR = 2.47 (95%CI 1.57-3.88; p < 0.01; I2=4%), as was the clinical response [OR 1.99 (95% CI 1.18-3.34; p=0.01; I2= 26%)]. There was an overall improvement in CRP [MD: -2.69 (95% CI -3.78,-1.60); p< 0.01; I2=0%) However, there was no significant difference in endoscopic remission between the two groups. [OR 1.89 (95%CI 0.93-3.83; p=0.08; I2=15%)]. Pooled adverse effects such as worsening colitis were comparable between the two groups. [OR 0.75 (95% CI 0.38-1.48; p=0.40; I2=0%)]. On subgroup analysis with respect to type of IBD, improved clinical remission was seen with UC [OR 2.60 (95% CI 1.63-4.15); p < 0.01;I2= 0%) but was not significant with CD [OR 2.26 (95% CI 0.25-20.12); p < 0.46;I2= 58%)]. Clinical response was improved with IMT in UC [OR 2.04 (95% CI 1.14-3.62); p < 0.02;I2= 34%)] and not CD. [OR 1.33 (95% CI 0.24-7.28); p < 0.46;I2= 58%)]
Discussion: This meta-analysis demonstrated a significant difference with higher odds of clinical remission and clinical response in IBD patients receiving IMT when compared to standard treatment.
There was no significant difference in endoscopic remission or adverse events (worsening colitis). Further large-scale RCTs are needed for a more comprehensive understanding of the benefits and efficacy of IMT in IBD, and data is needed to help stratify the patient population who would benefit the most from IMT.
Disclosures:
Ifrah Fatima, MD1, Jagadish Koyi, MD1, Ben Ponvilawan, MD2, Vineel Mallavarapu, 3, Babu Mohan, MD, MS4. P3624 - Intestinal Microbiota Transplant vs Standard Management in Patients With Inflammatory Bowel Disease: Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Missouri-Kansas City, Kansas City, MO; 2UMKC School of Medicine, Kansas City, MO; 3Carver College of Medicine, University of Iowa, Iowa City, IA; 4University of Utah Health School of Medicine, Salt Lake City, UT
Introduction: The role and clinical indications of Intestinal microbiota transplant (IMT) have witnessed increasing interest owing to advancements in disease process research and its role in dysbiosis. Several clinical trials administering IMT in patients with Ulcerative Colitis (UC) or Crohn's disease (CD) are directed towards the restoration and homeostasis of gut microbiome.
Methods: Six databases (Pubmed, Scopus, Embase, Medline, Web of Science, CCRCT) were screened from inception until March 2023. The search utilized relevant keywords and MeSH terms to include studies that evaluated the efficacy and safety of intestinal material transplant in IBD. Outcomes of interest included clinical response, clinical and endoscopic remission.
Standard meta-analysis methodology was followed using the random-effects model, and heterogeneity was assessed by I2 statistics.
Results: A total of 10 RCTs of patients were included in the final analysis. The combined mean age in the IMT vs control groups was 39.92±14.61 vs 35.2.±12.1 years. 83.2% of patients had UC vs 16.8% had CD.
The pooled OR for clinical remission was favorable with IMT, OR = 2.47 (95%CI 1.57-3.88; p < 0.01; I2=4%), as was the clinical response [OR 1.99 (95% CI 1.18-3.34; p=0.01; I2= 26%)]. There was an overall improvement in CRP [MD: -2.69 (95% CI -3.78,-1.60); p< 0.01; I2=0%) However, there was no significant difference in endoscopic remission between the two groups. [OR 1.89 (95%CI 0.93-3.83; p=0.08; I2=15%)]. Pooled adverse effects such as worsening colitis were comparable between the two groups. [OR 0.75 (95% CI 0.38-1.48; p=0.40; I2=0%)]. On subgroup analysis with respect to type of IBD, improved clinical remission was seen with UC [OR 2.60 (95% CI 1.63-4.15); p < 0.01;I2= 0%) but was not significant with CD [OR 2.26 (95% CI 0.25-20.12); p < 0.46;I2= 58%)]. Clinical response was improved with IMT in UC [OR 2.04 (95% CI 1.14-3.62); p < 0.02;I2= 34%)] and not CD. [OR 1.33 (95% CI 0.24-7.28); p < 0.46;I2= 58%)]
Discussion: This meta-analysis demonstrated a significant difference with higher odds of clinical remission and clinical response in IBD patients receiving IMT when compared to standard treatment.
There was no significant difference in endoscopic remission or adverse events (worsening colitis). Further large-scale RCTs are needed for a more comprehensive understanding of the benefits and efficacy of IMT in IBD, and data is needed to help stratify the patient population who would benefit the most from IMT.
Disclosures:
Ifrah Fatima indicated no relevant financial relationships.
Jagadish Koyi indicated no relevant financial relationships.
Ben Ponvilawan indicated no relevant financial relationships.
Vineel Mallavarapu indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Ifrah Fatima, MD1, Jagadish Koyi, MD1, Ben Ponvilawan, MD2, Vineel Mallavarapu, 3, Babu Mohan, MD, MS4. P3624 - Intestinal Microbiota Transplant vs Standard Management in Patients With Inflammatory Bowel Disease: Systematic Review and Meta-Analysis of Randomized Controlled Trials, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
