Tuesday Poster Session
Category: General Endoscopy
P3400 - Yield of Terminal Ileal Intubation in Evaluating Iron Deficiency Anemia
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Samantha Chua, MD
Boston University Medical Center
Boston, Massachusetts
Presenting Author(s)
Samantha Chua, MD, Max Rosenthaler, MD, Marcel Yibirin Wakim, MD, Christopher Huang, MD, James Connolly, MD, Laura Chiu, MD, MPH
Boston University Medical Center, Boston, MA
Introduction: Current guidelines recommend that patients with iron deficiency anemia (IDA) be considered for bidirectional endoscopy. Heterogeneity in performing terminal ileum (TI) intubation exists among endoscopists when evaluating IDA, and the incremental yield of this maneuver is unknown. We investigated the diagnostic yield of TI intubation during the workup of IDA within a diverse, safety-net hospital population.
Methods: We performed a single-center, retrospective cohort study of patients who underwent ileocolonoscopy for IDA evaluation between 1/1/2012 – 1/1/2022. Patients with inadequate bowel preparation and incomplete procedures were excluded (n=6). Demographic, clinical, endoscopic and histopathological finding characteristics were identified and examined in bivariate analyses.
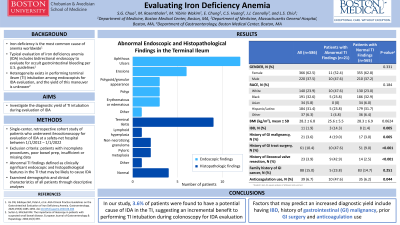
Results: Of the 2225 patients who underwent colonoscopy for IDA during the study period, a total of 586 patients (mean age 53.2 ± 15.4, 62.5% women) who completed ileocolonoscopy (26.3%) were included in our analyses. The descriptive characteristics of these patients and analysis by TI abnormality finding status are shown in Table 1. Twenty-one patients (3.6%) had abnormal endoscopic or histopathologic findings detected in the TI (Table 2). The most common findings were aphthous ulcers and erosions. No malignancy was found in any patient. The study cohort was predominantly English-speaking (59.6%) and had public insurance (72.9%). More than half the patients reported no history of tobacco use (61.3%) or alcohol use (67.7%). Patients with abnormal TI findings were more likely to have IBD (14.3% vs 1.4%, p = 0.005), history of gastrointestinal cancer (19% vs 3.0%, p = 0.005), history of gastrointestinal surgery (47.6% vs 9.0%, p < 0.001), prior ileocecal valve resection (42.9% vs 2.5%, p < 0.001), and anticoagulation use (19% vs 6.2%, p = 0.044).
Discussion: Potential endoscopic and histopathologic etiologies of IDA were found in approximately 4% of patients, suggesting a small incremental benefit to performing TI intubation routinely during colonoscopy for IDA evaluation. Having IBD, history of gastrointestinal cancer, prior gastrointestinal surgery and anticoagulation use were strongly associated with having TI abnormalities on ileocolonoscopy, and may therefore predict an increased diagnostic yield. Further research is needed to fully define the potential relationship between clinical patient characteristics and abnormal TI findings in the endoscopic investigation of IDA.

Disclosures:
Samantha Chua, MD, Max Rosenthaler, MD, Marcel Yibirin Wakim, MD, Christopher Huang, MD, James Connolly, MD, Laura Chiu, MD, MPH. P3400 - Yield of Terminal Ileal Intubation in Evaluating Iron Deficiency Anemia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Boston University Medical Center, Boston, MA
Introduction: Current guidelines recommend that patients with iron deficiency anemia (IDA) be considered for bidirectional endoscopy. Heterogeneity in performing terminal ileum (TI) intubation exists among endoscopists when evaluating IDA, and the incremental yield of this maneuver is unknown. We investigated the diagnostic yield of TI intubation during the workup of IDA within a diverse, safety-net hospital population.
Methods: We performed a single-center, retrospective cohort study of patients who underwent ileocolonoscopy for IDA evaluation between 1/1/2012 – 1/1/2022. Patients with inadequate bowel preparation and incomplete procedures were excluded (n=6). Demographic, clinical, endoscopic and histopathological finding characteristics were identified and examined in bivariate analyses.
Results: Of the 2225 patients who underwent colonoscopy for IDA during the study period, a total of 586 patients (mean age 53.2 ± 15.4, 62.5% women) who completed ileocolonoscopy (26.3%) were included in our analyses. The descriptive characteristics of these patients and analysis by TI abnormality finding status are shown in Table 1. Twenty-one patients (3.6%) had abnormal endoscopic or histopathologic findings detected in the TI (Table 2). The most common findings were aphthous ulcers and erosions. No malignancy was found in any patient. The study cohort was predominantly English-speaking (59.6%) and had public insurance (72.9%). More than half the patients reported no history of tobacco use (61.3%) or alcohol use (67.7%). Patients with abnormal TI findings were more likely to have IBD (14.3% vs 1.4%, p = 0.005), history of gastrointestinal cancer (19% vs 3.0%, p = 0.005), history of gastrointestinal surgery (47.6% vs 9.0%, p < 0.001), prior ileocecal valve resection (42.9% vs 2.5%, p < 0.001), and anticoagulation use (19% vs 6.2%, p = 0.044).
Discussion: Potential endoscopic and histopathologic etiologies of IDA were found in approximately 4% of patients, suggesting a small incremental benefit to performing TI intubation routinely during colonoscopy for IDA evaluation. Having IBD, history of gastrointestinal cancer, prior gastrointestinal surgery and anticoagulation use were strongly associated with having TI abnormalities on ileocolonoscopy, and may therefore predict an increased diagnostic yield. Further research is needed to fully define the potential relationship between clinical patient characteristics and abnormal TI findings in the endoscopic investigation of IDA.

Figure: Abnormal Endoscopic and Histopathological Terminal Ileum Findings
Disclosures:
Samantha Chua indicated no relevant financial relationships.
Max Rosenthaler indicated no relevant financial relationships.
Marcel Yibirin Wakim indicated no relevant financial relationships.
Christopher Huang indicated no relevant financial relationships.
James Connolly indicated no relevant financial relationships.
Laura Chiu indicated no relevant financial relationships.
Samantha Chua, MD, Max Rosenthaler, MD, Marcel Yibirin Wakim, MD, Christopher Huang, MD, James Connolly, MD, Laura Chiu, MD, MPH. P3400 - Yield of Terminal Ileal Intubation in Evaluating Iron Deficiency Anemia, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
