Tuesday Poster Session
Category: Stomach
P4212 - Gastric Glomus Tumor, Not a GIST
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Diana Lei Dy, RN, BSN
St. George's University School of Medicine
Las Vegas, NV
Presenting Author(s)
Diana Lei Dy, RN, BSN1, Michael Zimmerman, MD2
1St. George's University School of Medicine, Las Vegas, NV; 2Digestive Disease Specialists, Las Vegas, NV
Introduction: Glomus tumors are rare, benign neoplasms of mesenchymal cells, comprising 1-2% of all soft tissue tumors and predominantly found on the extremities. The GI tract is a rare site of incidence, but it most commonly involves the stomach, specifically, the antrum. These submucosal lesions are difficult to differentiate from other submucosal gastric neoplasms due to overlapping features. Thus, they are often mistaken for the more frequent GI stromal tumors (GIST). We describe a unique case of a gastric antral mass that was initially suspected as GIST, but then confirmed as a gastric glomus tumor (GGT).
Case Description/Methods: A 69-year-old Caucasian male with a past medical history of Barrett’s esophagus, chronic GERD and severe obesity presented with right-sided flank pain. Physical exam and labs were unremarkable. EGD showed a single localized non-bleeding nodule of benign appearance in the antrum, suggestive of a submucosal tumor (Fig A). CT A/P revealed an isolated mass in the lateral gastric wall with no invasion or metastasis. EUS showed a hypoechoic submucosal lesion in the antrum, measuring 2.25 x 1.1 cm and FNA revealed a spindle cell neoplasm, which was positive with smooth muscle actin (SMA), negative with CD117, CD34, S100, Desmin and BCL-2, and compatible with GIST. The patient underwent a partial gastrectomy. Post-operative course was uneventful and repeat EGD showed no recurrence. However, further histopathological findings of the resected mass revealed multiple nodules of tumor involving the gastric muscularis propria and subserosa, composed of round cells arranged in nests and sheets around thin-walled vessels, a calcified hyalinized nodule within the tumor and positive for SMA and BCL-2 with no evidence of atypical mitoses or necrosis (Fig B&C). Subsequently, a definitive diagnosis of GGT was made.
Discussion: GGTs originate from the neuromyoarterial glomus body and constitute < 1% of all GI soft tissue neoplasms. The non-specific patient presentation (e.g. abdominal pain, hematemesis) and lack of distinctive characteristics make it very difficult to differentiate from GIST preoperatively via endoscopy or imaging. In this case, multiple diagnostic modalities—EGD, CT A/P, EUS/FNA, surgical resection and 2 histopath analyses—were utilized to arrive at a definitive diagnosis. Albeit rare, it also has a malignant potential, which can change the course of patient management. Therefore, it is important to consider GGTs in the differential diagnosis of submucosal gastric tumors.

Disclosures:
Diana Lei Dy, RN, BSN1, Michael Zimmerman, MD2. P4212 - Gastric Glomus Tumor, Not a GIST, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1St. George's University School of Medicine, Las Vegas, NV; 2Digestive Disease Specialists, Las Vegas, NV
Introduction: Glomus tumors are rare, benign neoplasms of mesenchymal cells, comprising 1-2% of all soft tissue tumors and predominantly found on the extremities. The GI tract is a rare site of incidence, but it most commonly involves the stomach, specifically, the antrum. These submucosal lesions are difficult to differentiate from other submucosal gastric neoplasms due to overlapping features. Thus, they are often mistaken for the more frequent GI stromal tumors (GIST). We describe a unique case of a gastric antral mass that was initially suspected as GIST, but then confirmed as a gastric glomus tumor (GGT).
Case Description/Methods: A 69-year-old Caucasian male with a past medical history of Barrett’s esophagus, chronic GERD and severe obesity presented with right-sided flank pain. Physical exam and labs were unremarkable. EGD showed a single localized non-bleeding nodule of benign appearance in the antrum, suggestive of a submucosal tumor (Fig A). CT A/P revealed an isolated mass in the lateral gastric wall with no invasion or metastasis. EUS showed a hypoechoic submucosal lesion in the antrum, measuring 2.25 x 1.1 cm and FNA revealed a spindle cell neoplasm, which was positive with smooth muscle actin (SMA), negative with CD117, CD34, S100, Desmin and BCL-2, and compatible with GIST. The patient underwent a partial gastrectomy. Post-operative course was uneventful and repeat EGD showed no recurrence. However, further histopathological findings of the resected mass revealed multiple nodules of tumor involving the gastric muscularis propria and subserosa, composed of round cells arranged in nests and sheets around thin-walled vessels, a calcified hyalinized nodule within the tumor and positive for SMA and BCL-2 with no evidence of atypical mitoses or necrosis (Fig B&C). Subsequently, a definitive diagnosis of GGT was made.
Discussion: GGTs originate from the neuromyoarterial glomus body and constitute < 1% of all GI soft tissue neoplasms. The non-specific patient presentation (e.g. abdominal pain, hematemesis) and lack of distinctive characteristics make it very difficult to differentiate from GIST preoperatively via endoscopy or imaging. In this case, multiple diagnostic modalities—EGD, CT A/P, EUS/FNA, surgical resection and 2 histopath analyses—were utilized to arrive at a definitive diagnosis. Albeit rare, it also has a malignant potential, which can change the course of patient management. Therefore, it is important to consider GGTs in the differential diagnosis of submucosal gastric tumors.

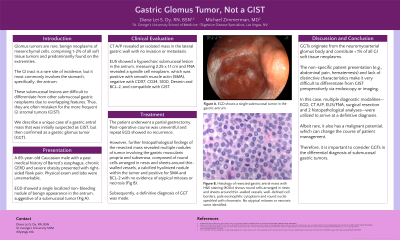
Figure: A. Esophagogastroduodenoscopy (EGD) shows a single submucosal tumor in the gastric antrum.
B. Histology of resected gastric antral mass with H&E staining (10x)
C. Histology of resected gastric antral mass with H&E staining (400x) shows round cells arranged in nests and sheets around thin-walled vessels, well-defined cell borders, pale eosinophilic cytoplasm and round nuclei speckled with chromatin. No atypical mitoses or necrosis were identified.
B. Histology of resected gastric antral mass with H&E staining (10x)
C. Histology of resected gastric antral mass with H&E staining (400x) shows round cells arranged in nests and sheets around thin-walled vessels, well-defined cell borders, pale eosinophilic cytoplasm and round nuclei speckled with chromatin. No atypical mitoses or necrosis were identified.
Disclosures:
Diana Lei Dy indicated no relevant financial relationships.
Michael Zimmerman indicated no relevant financial relationships.
Diana Lei Dy, RN, BSN1, Michael Zimmerman, MD2. P4212 - Gastric Glomus Tumor, Not a GIST, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
