Tuesday Poster Session
Category: Colorectal Cancer Prevention
P3215 - A Rare Case of Anorectal Melanoma
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Michelle Bernshteyn, MD
Guthrie Robert Packer Hospital
Sayre, PA
Presenting Author(s)
Michelle Bernshteyn, MD, Leonard Walsh, MD, Subash Ghimire, MD, Hani Hojjati, MD, Thomas McDonald, MD
Guthrie Robert Packer Hospital, Sayre, PA
Introduction: Anorectal melanoma occurs in 1-3% of melanoma. 68-year-old male underwent a colonoscopy and had a lesion on retroflexion determined to be malignant melanoma. Our case highlights the importance of retroflexion for complete evaluation
Case Description/Methods: An asymptomatic 68-year-old male with history of basal cell carcinoma presented for colonoscopy showing a distal rectal mucosal nodule on retroflexion. Biopsy revealed malignant melanoma infiltrating colonic mucosa. Tumor cells were positive for S100, Melan-A, and Sox 10 but negative for synaptophysin, chromogranin, EMA, Ber-EP4, LCA, and CD34.
Colorectal surgery recommended local excision. Oncology recommended staging and local excision if this did not show extension beyond anus. The role of adjuvant systemic therapy will be based on imaging and BRAF testing.
Positron emission tomography scan showed a discrete focus of intense uptake in distal rectum/anorectal junction. The patient underwent trans-anal excision of anorectal melanoma and closure with endorectal advancement flap.
Discussion: Incidence of melanoma of the anorectum is 1-3% but is the third most common site affected by melanoma. The two most common include the epidermis and retina. Diagnosis of anal versus rectal melanoma is made based on location of lesion to anal verge. One review reported most lesions were polypoid helping to differentiate from a carcinoma.
Histologically, cell type, pigmentation, pattern of growth, and tumor relationship to squamous and columnar mucosa aids in diagnosis. Staining with s100, HMB-45, Melan-A, and vimentin are important. Melanotic transformation of cells from nerves leads to melanoma of the gastrointestinal tract with a higher occurrence in the anorectal region or originates from the melanocytes of the rectal epithelium.
There are no treatment guidelines. Wide local excision is favored to abdominoperineal resection. Regardless, the average prognosis is 15 months with 10-20% 5-year survival. Distal site involvement has a worse prognosis. Adjuvant immunotherapy may beneficial, but sufficient data measuring efficacy in cases outside of cutaneous melanoma is lacking. BRAF mutation frequency in anorectal melanoma is not well-documented. Radiation therapy does not improve survival.
Retroflexion is recommended as an important part of colonoscopy. It increases detection of flat malignancies which can be overlooked with antegrade viewing. Risk of perforation during this maneuver should be considered. It is reported in 1.02 out of 10,000 procedures.

Disclosures:
Michelle Bernshteyn, MD, Leonard Walsh, MD, Subash Ghimire, MD, Hani Hojjati, MD, Thomas McDonald, MD. P3215 - A Rare Case of Anorectal Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Guthrie Robert Packer Hospital, Sayre, PA
Introduction: Anorectal melanoma occurs in 1-3% of melanoma. 68-year-old male underwent a colonoscopy and had a lesion on retroflexion determined to be malignant melanoma. Our case highlights the importance of retroflexion for complete evaluation
Case Description/Methods: An asymptomatic 68-year-old male with history of basal cell carcinoma presented for colonoscopy showing a distal rectal mucosal nodule on retroflexion. Biopsy revealed malignant melanoma infiltrating colonic mucosa. Tumor cells were positive for S100, Melan-A, and Sox 10 but negative for synaptophysin, chromogranin, EMA, Ber-EP4, LCA, and CD34.
Colorectal surgery recommended local excision. Oncology recommended staging and local excision if this did not show extension beyond anus. The role of adjuvant systemic therapy will be based on imaging and BRAF testing.
Positron emission tomography scan showed a discrete focus of intense uptake in distal rectum/anorectal junction. The patient underwent trans-anal excision of anorectal melanoma and closure with endorectal advancement flap.
Discussion: Incidence of melanoma of the anorectum is 1-3% but is the third most common site affected by melanoma. The two most common include the epidermis and retina. Diagnosis of anal versus rectal melanoma is made based on location of lesion to anal verge. One review reported most lesions were polypoid helping to differentiate from a carcinoma.
Histologically, cell type, pigmentation, pattern of growth, and tumor relationship to squamous and columnar mucosa aids in diagnosis. Staining with s100, HMB-45, Melan-A, and vimentin are important. Melanotic transformation of cells from nerves leads to melanoma of the gastrointestinal tract with a higher occurrence in the anorectal region or originates from the melanocytes of the rectal epithelium.
There are no treatment guidelines. Wide local excision is favored to abdominoperineal resection. Regardless, the average prognosis is 15 months with 10-20% 5-year survival. Distal site involvement has a worse prognosis. Adjuvant immunotherapy may beneficial, but sufficient data measuring efficacy in cases outside of cutaneous melanoma is lacking. BRAF mutation frequency in anorectal melanoma is not well-documented. Radiation therapy does not improve survival.
Retroflexion is recommended as an important part of colonoscopy. It increases detection of flat malignancies which can be overlooked with antegrade viewing. Risk of perforation during this maneuver should be considered. It is reported in 1.02 out of 10,000 procedures.

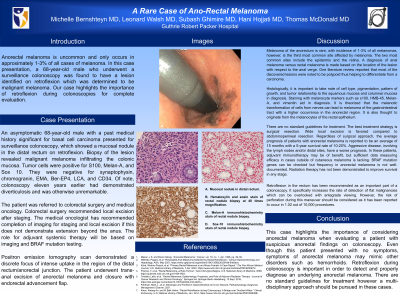
Figure: A. Hematoxylin and eosin stain of rectal nodule biopsy at 40 times magnification.
B. Melan-A immunohistochemistry stain of rectal nodule biopsy.
C. Sox-10 immunohistochemistry stain of rectal nodule biopsy.
B. Melan-A immunohistochemistry stain of rectal nodule biopsy.
C. Sox-10 immunohistochemistry stain of rectal nodule biopsy.
Disclosures:
Michelle Bernshteyn indicated no relevant financial relationships.
Leonard Walsh indicated no relevant financial relationships.
Subash Ghimire indicated no relevant financial relationships.
Hani Hojjati indicated no relevant financial relationships.
Thomas McDonald indicated no relevant financial relationships.
Michelle Bernshteyn, MD, Leonard Walsh, MD, Subash Ghimire, MD, Hani Hojjati, MD, Thomas McDonald, MD. P3215 - A Rare Case of Anorectal Melanoma, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
