Tuesday Poster Session
Category: Stomach
P4215 - Peri-Gastric Abscess of Unknown Origin
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Kavea Panneerselvam, MD
University of Texas Health Science Center at San Antonio
San Antonio, TX
Presenting Author(s)
Kavea Panneerselvam, MD1, Mahesh Gajendran, MD, MPH1, Priyadarshini Loganathan, MD2, Edgar R. Infante, MD1, Laura Rosenkranz, MD1
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX
Introduction: Peri-gastric abscesses are rare and usually occur as a result of malignancy, instrumentation, or surgery. Here, we present a case of a spontaneous peri-gastric abscess in a patient with diabetes.
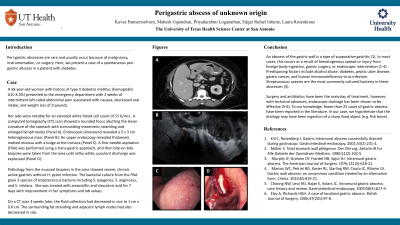
Case Description/Methods: A 58-year-old woman with history of type II diabetes mellitus (hemoglobin A1C 8.3%) presented to the emergency department with 2 weeks of intermittent left-sided abdominal pain associated with nausea, decreased oral intake, and weight loss of 9 pounds. Her labs were notable for an elevated white blood cell count of 15 K/mcL. A computed tomography (CT) scan showed a rounded focus abutting the lesser curvature of the stomach with surrounding mesenteric stranding and enlarged lymph nodes (Panel A). Endoscopic ultrasound revealed a 5 x 3 cm heterogeneous mass (Panel B). An upper endoscopy revealed thickened, matted mucosa with a bulge at the incisura (Panel C). Fine-needle aspiration (FNA) was performed using a trans-gastric approach, and then bite-on-bite biopsies were taken from the area until milky white, purulent discharge was expressed (Panel D). Pathology from the mucosal biopsies in the area showed severe, chronic active gastritis without H. pylori infection. The bacterial culture from the FNA grew 3 species of streptococcus bacteria including S. pyogenes, S. anginosus, and S. viridans. She was treated with amoxicillin and clavulanic acid for 7 days with improvement in her symptoms and lab values. On a CT scan 3 weeks later, the fluid collection had decreased in size to 1 cm x 0.6 cm. The surrounding fat stranding and adjacent lymph nodes had also decreased in size.
Discussion: An abscess of the gastric wall is a type of suppurative gastritis. In most cases, this occurs as a result of hematogenous spread or injury from foreign body ingestion, gastric surgery, or endoscopic intervention. Predisposing factors include alcohol abuse, diabetes, peptic ulcer disease, gastric cancer, and human immunodeficiency virus infection. Streptococcus species are the most commonly cultured bacteria in these abscesses. Surgery and antibiotics have been the mainstay of treatment, however, with technical advances, endoscopic drainage has been shown to be effective. To our knowledge, fewer than 25 cases of gastric abscess have been reported in the literature. In our case, we hypothesize that the etiology may have been ingestion of a sharp food object (e.g. fish bone).

Disclosures:
Kavea Panneerselvam, MD1, Mahesh Gajendran, MD, MPH1, Priyadarshini Loganathan, MD2, Edgar R. Infante, MD1, Laura Rosenkranz, MD1. P4215 - Peri-Gastric Abscess of Unknown Origin, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Texas Health Science Center at San Antonio, San Antonio, TX; 2University of Texas Health Science Center, San Antonio, TX
Introduction: Peri-gastric abscesses are rare and usually occur as a result of malignancy, instrumentation, or surgery. Here, we present a case of a spontaneous peri-gastric abscess in a patient with diabetes.
Case Description/Methods: A 58-year-old woman with history of type II diabetes mellitus (hemoglobin A1C 8.3%) presented to the emergency department with 2 weeks of intermittent left-sided abdominal pain associated with nausea, decreased oral intake, and weight loss of 9 pounds. Her labs were notable for an elevated white blood cell count of 15 K/mcL. A computed tomography (CT) scan showed a rounded focus abutting the lesser curvature of the stomach with surrounding mesenteric stranding and enlarged lymph nodes (Panel A). Endoscopic ultrasound revealed a 5 x 3 cm heterogeneous mass (Panel B). An upper endoscopy revealed thickened, matted mucosa with a bulge at the incisura (Panel C). Fine-needle aspiration (FNA) was performed using a trans-gastric approach, and then bite-on-bite biopsies were taken from the area until milky white, purulent discharge was expressed (Panel D). Pathology from the mucosal biopsies in the area showed severe, chronic active gastritis without H. pylori infection. The bacterial culture from the FNA grew 3 species of streptococcus bacteria including S. pyogenes, S. anginosus, and S. viridans. She was treated with amoxicillin and clavulanic acid for 7 days with improvement in her symptoms and lab values. On a CT scan 3 weeks later, the fluid collection had decreased in size to 1 cm x 0.6 cm. The surrounding fat stranding and adjacent lymph nodes had also decreased in size.
Discussion: An abscess of the gastric wall is a type of suppurative gastritis. In most cases, this occurs as a result of hematogenous spread or injury from foreign body ingestion, gastric surgery, or endoscopic intervention. Predisposing factors include alcohol abuse, diabetes, peptic ulcer disease, gastric cancer, and human immunodeficiency virus infection. Streptococcus species are the most commonly cultured bacteria in these abscesses. Surgery and antibiotics have been the mainstay of treatment, however, with technical advances, endoscopic drainage has been shown to be effective. To our knowledge, fewer than 25 cases of gastric abscess have been reported in the literature. In our case, we hypothesize that the etiology may have been ingestion of a sharp food object (e.g. fish bone).

Figure: Panel A: CT image showing a peri-gastric fluid collection. Panel B: 5 cm x 3 cm heterogeneous mass abutting the incisura seen on endoscopic ultrasound. Panel C: Thickened, matted mucosa at the incisura, seen on endoscopy. Panel D: Purulent discharge expressed from the incisura after bite-on-bite biopsies were taken to disrupt the mucosa.
Disclosures:
Kavea Panneerselvam indicated no relevant financial relationships.
Mahesh Gajendran indicated no relevant financial relationships.
Priyadarshini Loganathan indicated no relevant financial relationships.
Edgar Infante indicated no relevant financial relationships.
Laura Rosenkranz indicated no relevant financial relationships.
Kavea Panneerselvam, MD1, Mahesh Gajendran, MD, MPH1, Priyadarshini Loganathan, MD2, Edgar R. Infante, MD1, Laura Rosenkranz, MD1. P4215 - Peri-Gastric Abscess of Unknown Origin, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
