Tuesday Poster Session
Category: Stomach
P4217 - A Case of Severe Gastroparesis in a Patient With Metastatic Breast Cancer Secondary to Capecitabine Therapy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Vineela Appalaneni, MD
Loyola University Medical Center
Maywood, IL
Presenting Author(s)
Vineela Appalaneni, MD, Peter Sargon, MD, Zuie Wakade, DO, Sana Gafoor, DO, Abdul Haseeb, MD
Loyola University Medical Center, Maywood, IL
Introduction: Gastroparesis (GP) is a motility disorder defined by delayed gastric emptying in the absence of mechanical outlet obstruction. Numerous etiologies have been identified for GP, but up to half of cases are idiopathic. We present a case of gastroparesis secondary to capecitabine therapy.
Case Description/Methods: A 78-year-old female with recurrent metastatic breast cancer presented to the ED with persistent nausea and vomiting. She had been undergoing various treatments for breast cancer for the past 7 years, with most recent therapy being oral capecitabine. CT scan showed a significantly distended stomach without evidence of obstruction or a transition point. She went for upper endoscopy and endoscopic ultrasound the next day which revealed a large, distorted stomach as well as proximal jejunal stenosis without any masses noted. Biopsies from EGD showed findings of normal duodenal mucosa and mild reactive gastropathy. This constellation of findings was attributed to gastroparesis secondary to capecitabine therapy. Despite nasogastric tube (NGT) decompression and resultant significant output through NGT along with initiation of metoclopramide for aiding motility, patient experienced minimal relief. She had to maintain prolonged NPO status due to her inability to tolerate an enteral diet. Total parenteral nutrition (TPN) was initiated after 5 days of complete NPO status. PEG-J tube was eventually placed during hospitalization; however, tube feedings were limited by ongoing abdominal distension and pain. She had to restart TPN and was discharged home with TPN for complete nutrition. Ongoing course was complicated by severe hypernatremia and dehydration requiring admission to the intensive care unit. Given ongoing critical issues with nutrition as well as overall poor performance status, the patient transitioned to comfort care and was discharged with home hospice with a liberalized diet for pleasure. She subsequently passed away a few weeks later.
Discussion: Capecitabine-induced visceral neuropathy can lead to severe gastroparesis and poor quality of life in patients if it goes unrecognized. Higher clinical suspicion and vigilance are needed by gastroenterologists in diagnosing this unusual adverse effect, especially with increasing oral capecitabine use.

Disclosures:
Vineela Appalaneni, MD, Peter Sargon, MD, Zuie Wakade, DO, Sana Gafoor, DO, Abdul Haseeb, MD. P4217 - A Case of Severe Gastroparesis in a Patient With Metastatic Breast Cancer Secondary to Capecitabine Therapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Loyola University Medical Center, Maywood, IL
Introduction: Gastroparesis (GP) is a motility disorder defined by delayed gastric emptying in the absence of mechanical outlet obstruction. Numerous etiologies have been identified for GP, but up to half of cases are idiopathic. We present a case of gastroparesis secondary to capecitabine therapy.
Case Description/Methods: A 78-year-old female with recurrent metastatic breast cancer presented to the ED with persistent nausea and vomiting. She had been undergoing various treatments for breast cancer for the past 7 years, with most recent therapy being oral capecitabine. CT scan showed a significantly distended stomach without evidence of obstruction or a transition point. She went for upper endoscopy and endoscopic ultrasound the next day which revealed a large, distorted stomach as well as proximal jejunal stenosis without any masses noted. Biopsies from EGD showed findings of normal duodenal mucosa and mild reactive gastropathy. This constellation of findings was attributed to gastroparesis secondary to capecitabine therapy. Despite nasogastric tube (NGT) decompression and resultant significant output through NGT along with initiation of metoclopramide for aiding motility, patient experienced minimal relief. She had to maintain prolonged NPO status due to her inability to tolerate an enteral diet. Total parenteral nutrition (TPN) was initiated after 5 days of complete NPO status. PEG-J tube was eventually placed during hospitalization; however, tube feedings were limited by ongoing abdominal distension and pain. She had to restart TPN and was discharged home with TPN for complete nutrition. Ongoing course was complicated by severe hypernatremia and dehydration requiring admission to the intensive care unit. Given ongoing critical issues with nutrition as well as overall poor performance status, the patient transitioned to comfort care and was discharged with home hospice with a liberalized diet for pleasure. She subsequently passed away a few weeks later.
Discussion: Capecitabine-induced visceral neuropathy can lead to severe gastroparesis and poor quality of life in patients if it goes unrecognized. Higher clinical suspicion and vigilance are needed by gastroenterologists in diagnosing this unusual adverse effect, especially with increasing oral capecitabine use.

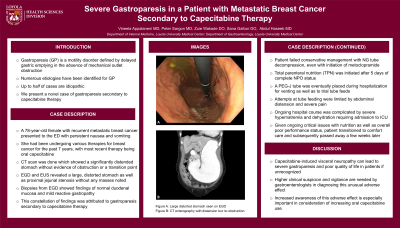
Figure: Figure A: Large distorted stomach seen on EGD
Figure B: CT enterography
Figure B: CT enterography
Disclosures:
Vineela Appalaneni indicated no relevant financial relationships.
Peter Sargon indicated no relevant financial relationships.
Zuie Wakade indicated no relevant financial relationships.
Sana Gafoor indicated no relevant financial relationships.
Abdul Haseeb indicated no relevant financial relationships.
Vineela Appalaneni, MD, Peter Sargon, MD, Zuie Wakade, DO, Sana Gafoor, DO, Abdul Haseeb, MD. P4217 - A Case of Severe Gastroparesis in a Patient With Metastatic Breast Cancer Secondary to Capecitabine Therapy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
