Tuesday Poster Session
Category: Endoscopy Video Forum
P3221 - Sub-Mucosal Tunneling Endoscopic Resection for Management of a Rare Case of Esophageal Gastrointestinal Stromal Tumor

Chukwunonso B. Ezeani, MBBS
Baton Rouge General Hospital
Baton Rouge, LA
Presenting Author(s)
1Baton Rouge General Hospital, Baton Rouge, LA; 2Beth Israel Deaconess Medical Center, Boston, MA; 3BIDMC, Boston, MA
Introduction:
Endoscopic Submucosal Dissection (ESD) is an established minimally invasive procedure for the removal of gastrointestinal lesions. Submucosal Tunneling Endoscopic resection (STER) is an emerging technique within the field of ESD that involves tunnel-exposed, endoscopic full-thickness resection. It is now widely favored treatment for tumors originating from the muscularis propria layer.
Gastrointestinal Stromal Tumors (GIST) are potentially malignant subepithelial mesenchymal tumors, rarely found in the esophagus. Treatment options include surveillance, surgical resection, and imatinib. We present a rare case of esophageal GIST successfully removed with STER
Case Description/Methods:
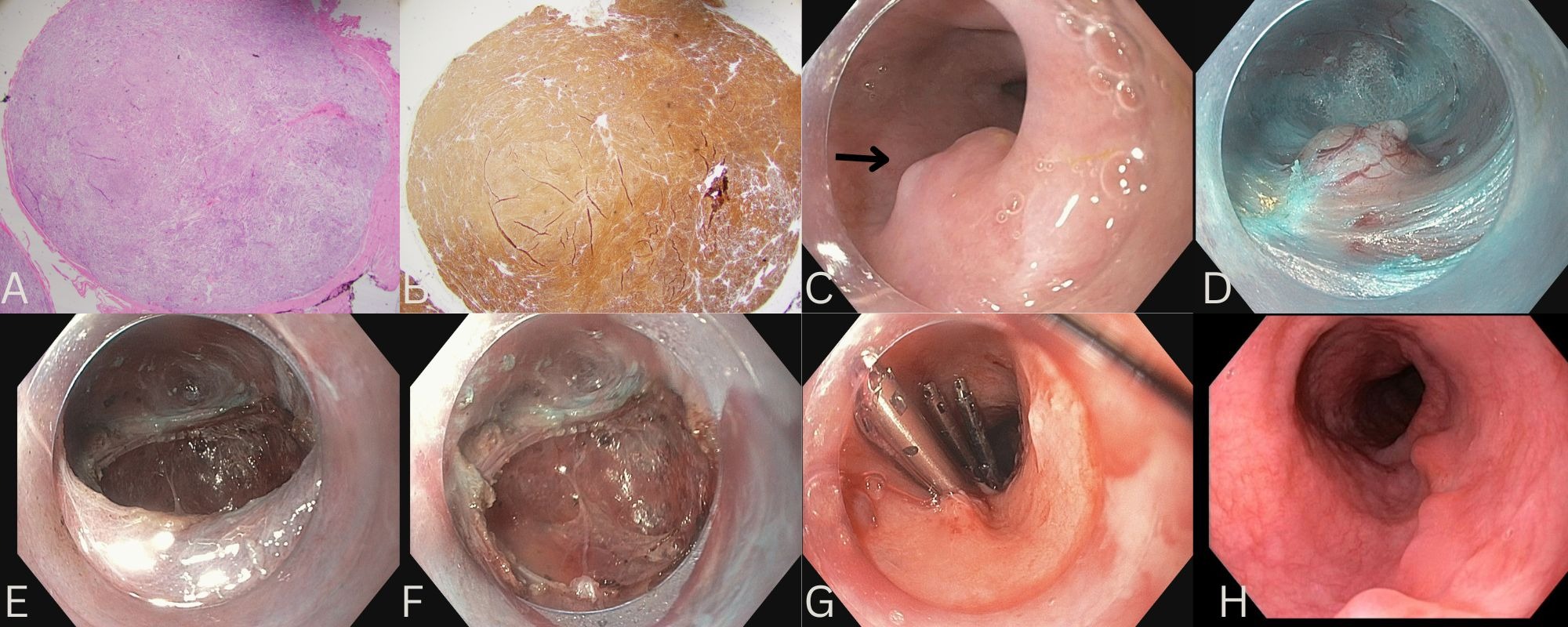
A 75-year-old woman with a history of compensated alcohol-related cirrhosis underwent upper endoscopy for variceal screening which revealed an incidental 1 cm well-circumscribed upper esophageal submucosal lesion. Endoscopic ultrasound revealed a 1 cm by 1 cm oval, homogenous, and hypoechoic mass in the upper esophagus, arising from the muscularis propria layer. Pathology from biopsies was consistent with GIST (A, B). The patient opted for endoscopic removal.
An injector force needle was used to create a large submucosal injection using a lifting agent proximal to the mass, a longitudinal mucosal incision was made using the electrocautery knife. Tunnel creation by submucosal dissection was then performed. The mass was identified originating from the muscularis propria layer (C, D). The tunnel was extended 2 cm distal to the mass. Resection of the mass was then performed. The mucosal surface was dissected beginning from anal to oral portion. The remaining attached bands of muscularis propria on the anal portion were resected ensuring complete endoscopic en-bloc resection. The specimen was retrieved and sent to pathology. The entire defect bed was inspected with no active bleeding noted (E, F). The mucosal defect was closed using hemoclips (G). She was monitored overnight and discharged in good condition. Follow-up EGD 4 weeks later revealed healed defect with scarring (H)
Discussion:
Our case highlights the utility of STER in the management of esophageal GIST with excellent clinical outcomes. STER is safe and achieves high complete resection rates, en bloc rates, low risk of perforation and allows for better wound healing, reduced GI tract leakage, hospital stay, and more precise hemostasis compared to surgical resection. Further prospective studies are needed to establish the role of STER in larger submucosal tumors
Disclosures:
Chukwunonso B. Ezeani, MBBS1, Samuel Igbinedion, MD2, Erik Holzwanger, MD2, Sultan Mahmood, MD2, Michael Kent, MD2, Mandeep Sawhney, MD, MS2, Douglas Pleskow, MD, FACG3, Tyler Berzin, MD, FACG2, Moamen Gabr, MD, MSc,2. P3221 - Sub-Mucosal Tunneling Endoscopic Resection for Management of a Rare Case of Esophageal Gastrointestinal Stromal Tumor, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
