Tuesday Poster Session
Category: Colon
P3117 - Case of Severe Multifactorial Diarrhea in the Setting of Clostridioides difficile; Infection and Lymphocytic Colitis Unresponsive to Budesonide
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Heather Gosnell, DO
University of South Florida Morsani College of Medicine
Tampa, FL
Presenting Author(s)
Heather Gosnell, DO1, Kristen Tessiatore, MD2, Shreya Narayanan, MD1
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida, Tampa, FL
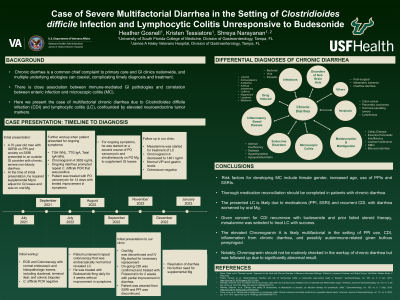
Introduction: There is close association between immune-mediated GI pathologies, and correlation between enteric infection and microscopic colitis. We present a case of multifactorial chronic diarrhea with Clostridioides difficile (C. diff) infection (CDI) and lymphocytic colitis (LC), confounded by elevated neuroendocrine tumor (NET) markers.
Case Description/Methods: A 70-year-old man with GERD and anxiety was evaluated at an outside clinic for chronic, severe non-bloody diarrhea requiring supplemental magnesium (Mg). Initial C. diff PCR was negative and EGD and colonoscopy showed normal mucosa without histopathologic signs of celiac, ileitis, or colitis. Further workup revealed Chromogranin A of 3835 ng/ml (normal < 311 ng/ml) with normal TSH, 24-hour urine 5-HIAA, celiac serologies, and contrasted abdominopelvic CT scans. C. diff PCR was repeated for ongoing diarrhea and was positive. He received 14 days of PO vancomycin without improvement then completed repeat colonoscopy with biopsy that revealed LC. He received budesonide 9 mg QD for four weeks and prednisone 20 mg BID for two weeks without relief. Four months later, C. diff PCR and toxin were repeated and positive. He again received 14 days of PO vancomycin without symptom resolution. He was then referred to our clinic.
On our initial evaluation, the diarrhea was partially managed with anti-diarrheal therapy. Anti-diarrheal agents, PPI, and SSRI were held. He was switched to IV Mg supplementation and was treated with fidaxomicin for recently positive C. diff. He then received mesalamine 3g daily for three months with complete resolution of both diarrhea and need for Mg supplementation. Workup for possible NET including labs and Octreoscan was negative, with notable drop in Chromogranin A on repeat testing. During this time, he was also diagnosed with bullous pemphigoid and latent TB.
Discussion: Thorough medication reconciliation should be completed in patients with chronic diarrhea. The presented LC is likely due to medications (PPI, SSRI) and recurrent CDI, with diarrhea worsened by oral Mg. Given concern for CDI recurrence with budesonide and prior failed steroid therapy, mesalamine was selected to treat LC with success. The elevated Chromogranin A is likely multifactorial in the setting of PPI use, CDI, inflammation from chronic diarrhea, and possibly autoimmune-related given bullous pemphigoid. Notably, Chromogranin should not be routinely checked in the workup of chronic diarrhea but was followed up due to significantly abnormal result.
Disclosures:
Heather Gosnell, DO1, Kristen Tessiatore, MD2, Shreya Narayanan, MD1. P3117 - Case of Severe Multifactorial Diarrhea in the Setting of Clostridioides difficile; Infection and Lymphocytic Colitis Unresponsive to Budesonide, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of South Florida Morsani College of Medicine, Tampa, FL; 2University of South Florida, Tampa, FL
Introduction: There is close association between immune-mediated GI pathologies, and correlation between enteric infection and microscopic colitis. We present a case of multifactorial chronic diarrhea with Clostridioides difficile (C. diff) infection (CDI) and lymphocytic colitis (LC), confounded by elevated neuroendocrine tumor (NET) markers.
Case Description/Methods: A 70-year-old man with GERD and anxiety was evaluated at an outside clinic for chronic, severe non-bloody diarrhea requiring supplemental magnesium (Mg). Initial C. diff PCR was negative and EGD and colonoscopy showed normal mucosa without histopathologic signs of celiac, ileitis, or colitis. Further workup revealed Chromogranin A of 3835 ng/ml (normal < 311 ng/ml) with normal TSH, 24-hour urine 5-HIAA, celiac serologies, and contrasted abdominopelvic CT scans. C. diff PCR was repeated for ongoing diarrhea and was positive. He received 14 days of PO vancomycin without improvement then completed repeat colonoscopy with biopsy that revealed LC. He received budesonide 9 mg QD for four weeks and prednisone 20 mg BID for two weeks without relief. Four months later, C. diff PCR and toxin were repeated and positive. He again received 14 days of PO vancomycin without symptom resolution. He was then referred to our clinic.
On our initial evaluation, the diarrhea was partially managed with anti-diarrheal therapy. Anti-diarrheal agents, PPI, and SSRI were held. He was switched to IV Mg supplementation and was treated with fidaxomicin for recently positive C. diff. He then received mesalamine 3g daily for three months with complete resolution of both diarrhea and need for Mg supplementation. Workup for possible NET including labs and Octreoscan was negative, with notable drop in Chromogranin A on repeat testing. During this time, he was also diagnosed with bullous pemphigoid and latent TB.
Discussion: Thorough medication reconciliation should be completed in patients with chronic diarrhea. The presented LC is likely due to medications (PPI, SSRI) and recurrent CDI, with diarrhea worsened by oral Mg. Given concern for CDI recurrence with budesonide and prior failed steroid therapy, mesalamine was selected to treat LC with success. The elevated Chromogranin A is likely multifactorial in the setting of PPI use, CDI, inflammation from chronic diarrhea, and possibly autoimmune-related given bullous pemphigoid. Notably, Chromogranin should not be routinely checked in the workup of chronic diarrhea but was followed up due to significantly abnormal result.
Disclosures:
Heather Gosnell indicated no relevant financial relationships.
Kristen Tessiatore indicated no relevant financial relationships.
Shreya Narayanan indicated no relevant financial relationships.
Heather Gosnell, DO1, Kristen Tessiatore, MD2, Shreya Narayanan, MD1. P3117 - Case of Severe Multifactorial Diarrhea in the Setting of Clostridioides difficile; Infection and Lymphocytic Colitis Unresponsive to Budesonide, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
