Tuesday Poster Session
Category: Small Intestine
P4121 - A Case of Duodenal Kaposi Sarcoma in a Patient With AIDS
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Bryce Kunkle, MD
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Bryce Kunkle, MD, Ahmad Al-Dwairy, MD, Kathryn Preacher, FNP, Obada Tabbaa, MD, Walid Chalhoub, MD
MedStar Georgetown University Hospital, Washington, DC
Introduction: Kaposi Sarcoma (KS) is a rare vascular tumor that is associated with Acquired Immunodeficiency Syndrome (AIDS) and can rarely cause mucosal lesions throughout the gastrointestinal (GI) tract. While often asymptomatic, GI KS can lead to a spectrum of presentations and is a poor prognostic indicator in patients with KS.
Case Description/Methods: A 40-year-old male with a past medical history of AIDS presented to our institution with two weeks duration of abdominal discomfort and anorexia. Initial workup was significant for multiple electrolyte abnormalities, CD4 count of 1, blood cultures positive for methicillin resistant Staphylococcus aureus (MRSA), and tricuspid vegetation visualized on trans-esophageal echocardiogram. The patient was admitted to the medical intensive care unit for septic shock and infective endocarditis.
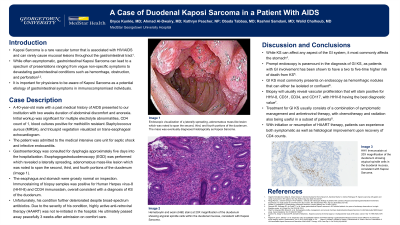
Gastroenterology was consulted for dysphagia approximately five days into the hospitalization. Esophagogastroduodenoscopy (EGD) was performed which revealed a laterally spreading, adenomatous mass-like lesion which was noted to span the second, third, and fourth portions of the duodenum (Image 1). The esophagus and stomach were grossly normal on inspection. Immuno-staining of biopsy samples was positive for Human Herpes virus-8 (HHV-8) and CD34 immuno-stain, overall consistent with a diagnosis of KS of the duodenum. Unfortunately, his condition further deteriorated despite broad-spectrum antibiotics. Due to the severity of his condition, highly active anti-retroviral therapy (HAART) was not re-initiated in the hospital. He ultimately passed away peacefully 3 weeks after admission on comfort care.
Discussion: While KS can affect any aspect of the GI system, it most commonly affects the stomach. Prompt endoscopy is paramount in the diagnosis of GI KS, as patients with GI involvement has been shown to have a two to five-time higher risk of death from KS. GI KS most commonly presents on endoscopy as hemorrhagic nodules that can either be isolated or confluent. Biopsy will usually reveal vascular proliferation that will stain positive for HHV-8, CD31, CD34, and CD117, with HHV-8 having the best diagnostic value.
Treatment for GI KS usually consists of a combination of symptomatic management and antiretroviral therapy, with chemotherapy and radiation also being useful in a subset of patients. With initiation or resumption of HAART therapy, patients can experience both symptomatic as well as histological improvement upon recovery of CD4 counts.

Disclosures:
Bryce Kunkle, MD, Ahmad Al-Dwairy, MD, Kathryn Preacher, FNP, Obada Tabbaa, MD, Walid Chalhoub, MD. P4121 - A Case of Duodenal Kaposi Sarcoma in a Patient With AIDS, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
MedStar Georgetown University Hospital, Washington, DC
Introduction: Kaposi Sarcoma (KS) is a rare vascular tumor that is associated with Acquired Immunodeficiency Syndrome (AIDS) and can rarely cause mucosal lesions throughout the gastrointestinal (GI) tract. While often asymptomatic, GI KS can lead to a spectrum of presentations and is a poor prognostic indicator in patients with KS.
Case Description/Methods: A 40-year-old male with a past medical history of AIDS presented to our institution with two weeks duration of abdominal discomfort and anorexia. Initial workup was significant for multiple electrolyte abnormalities, CD4 count of 1, blood cultures positive for methicillin resistant Staphylococcus aureus (MRSA), and tricuspid vegetation visualized on trans-esophageal echocardiogram. The patient was admitted to the medical intensive care unit for septic shock and infective endocarditis.
Gastroenterology was consulted for dysphagia approximately five days into the hospitalization. Esophagogastroduodenoscopy (EGD) was performed which revealed a laterally spreading, adenomatous mass-like lesion which was noted to span the second, third, and fourth portions of the duodenum (Image 1). The esophagus and stomach were grossly normal on inspection. Immuno-staining of biopsy samples was positive for Human Herpes virus-8 (HHV-8) and CD34 immuno-stain, overall consistent with a diagnosis of KS of the duodenum. Unfortunately, his condition further deteriorated despite broad-spectrum antibiotics. Due to the severity of his condition, highly active anti-retroviral therapy (HAART) was not re-initiated in the hospital. He ultimately passed away peacefully 3 weeks after admission on comfort care.
Discussion: While KS can affect any aspect of the GI system, it most commonly affects the stomach. Prompt endoscopy is paramount in the diagnosis of GI KS, as patients with GI involvement has been shown to have a two to five-time higher risk of death from KS. GI KS most commonly presents on endoscopy as hemorrhagic nodules that can either be isolated or confluent. Biopsy will usually reveal vascular proliferation that will stain positive for HHV-8, CD31, CD34, and CD117, with HHV-8 having the best diagnostic value.
Treatment for GI KS usually consists of a combination of symptomatic management and antiretroviral therapy, with chemotherapy and radiation also being useful in a subset of patients. With initiation or resumption of HAART therapy, patients can experience both symptomatic as well as histological improvement upon recovery of CD4 counts.

Figure: Endoscopic visualization of a laterally spreading, adenomatous mass-like lesion which was noted to span the second, third, and fourth portions of the duodenum. The mass was eventually diagnosed histologically as Kaposi Sarcoma.
Disclosures:
Bryce Kunkle indicated no relevant financial relationships.
Ahmad Al-Dwairy indicated no relevant financial relationships.
Kathryn Preacher indicated no relevant financial relationships.
Obada Tabbaa indicated no relevant financial relationships.
Walid Chalhoub indicated no relevant financial relationships.
Bryce Kunkle, MD, Ahmad Al-Dwairy, MD, Kathryn Preacher, FNP, Obada Tabbaa, MD, Walid Chalhoub, MD. P4121 - A Case of Duodenal Kaposi Sarcoma in a Patient With AIDS, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
