Tuesday Poster Session
Category: Colon
P3005 - Predictors of Outcomes in Hospitalization for Diverticular Disease
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- KY
Kevin Yang, MD
University at Buffalo
Buffalo, NY
Presenting Author(s)
Kevin Yang, MD, Gregory D. Gudleski, PhD, Ali A.. Aijaz, DO, Omar Arman, MD, Corrine Kickel, MD, Nariman Hossein-Javaheri, DO, Alexander M. Carlson, DO, Matthew J.. Hudson, MD, Mayada Ismail, MD
University at Buffalo, Buffalo, NY
Introduction: Despite the growing prevalence of diverticulosis-related hospitalizations, identifying predictors of outcomes for these patients remains a challenge. We planned to describe factors that can help predict the course of hospitalizations for diverticular disease, in hopes of guiding treatment strategies and allocation of resources.
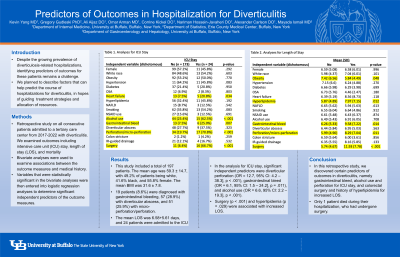
Methods: We designed a retrospective study on all consecutive patients admitted to a tertiary care center from 2017-2022 with complications related to diverticular disease, including diverticular bleeding, diverticulitis, abscesses, obstruction, and perforation. We documented demographic data, medical history, and clinical outcomes such as endoscopic intervention, surgery, interventional radiology-guided drainage, intensive care unit (ICU) stay, length of stay (LOS), and mortality. Bivariate analyses were used to examine associations between the outcome measures and demographic/medical history. Variables that were statistically significant in the bivariate analyses were then entered into logistic regression analyses to determine significant independent predictors of the outcome measures.
Results: This study included a total of 230 patients. The mean age was 60.8 (SD = 15), with 47.8% of patients being white, 44.3% black, 43% male, and 57% female. The mean BMI was 31.2 (SD = 7.9). 158 patients were diagnosed with diverticulitis, 52 with diverticular bleed, 68 with diverticular abscess, and 53 with micro-perforation/frank perforation. 27 patients were admitted to the ICU and 6 patients died during hospitalization. In the analysis examining mortality as the outcome, significant predictors were diverticular bleeding (OR = 15.8, 95% CI: 4.9 – 121.6], p < .001) and history of non-alcoholic fatty liver disease (NAFLD) (OR = 9.2, 95% CI: 1.5 – 85.0], p = .039). In the analysis for ICU admission, significant predictors were diverticular perforation (OR = 11.1, 95% CI: 3.9 – 31.9], p < .001), NAFLD (OR = 5.7, 95% CI: 1.4 – 22.6], p = .014), and alcohol use (OR = 3.9, 95% CI: 1.5 – 10.1], p = .005). Surgery (p < .001) and colonoscopies (p = .002) were associated with increased LOS.
Discussion: In this retrospective study, we discovered that admission for diverticular bleeding and history of NAFLD were associated with increased mortality. NAFLD, perforation, and alcohol use increased the risk for ICU stay, while longer LOS was seen for patients who underwent surgery or colonoscopy.
Disclosures:
Kevin Yang, MD, Gregory D. Gudleski, PhD, Ali A.. Aijaz, DO, Omar Arman, MD, Corrine Kickel, MD, Nariman Hossein-Javaheri, DO, Alexander M. Carlson, DO, Matthew J.. Hudson, MD, Mayada Ismail, MD. P3005 - Predictors of Outcomes in Hospitalization for Diverticular Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
University at Buffalo, Buffalo, NY
Introduction: Despite the growing prevalence of diverticulosis-related hospitalizations, identifying predictors of outcomes for these patients remains a challenge. We planned to describe factors that can help predict the course of hospitalizations for diverticular disease, in hopes of guiding treatment strategies and allocation of resources.
Methods: We designed a retrospective study on all consecutive patients admitted to a tertiary care center from 2017-2022 with complications related to diverticular disease, including diverticular bleeding, diverticulitis, abscesses, obstruction, and perforation. We documented demographic data, medical history, and clinical outcomes such as endoscopic intervention, surgery, interventional radiology-guided drainage, intensive care unit (ICU) stay, length of stay (LOS), and mortality. Bivariate analyses were used to examine associations between the outcome measures and demographic/medical history. Variables that were statistically significant in the bivariate analyses were then entered into logistic regression analyses to determine significant independent predictors of the outcome measures.
Results: This study included a total of 230 patients. The mean age was 60.8 (SD = 15), with 47.8% of patients being white, 44.3% black, 43% male, and 57% female. The mean BMI was 31.2 (SD = 7.9). 158 patients were diagnosed with diverticulitis, 52 with diverticular bleed, 68 with diverticular abscess, and 53 with micro-perforation/frank perforation. 27 patients were admitted to the ICU and 6 patients died during hospitalization. In the analysis examining mortality as the outcome, significant predictors were diverticular bleeding (OR = 15.8, 95% CI: 4.9 – 121.6], p < .001) and history of non-alcoholic fatty liver disease (NAFLD) (OR = 9.2, 95% CI: 1.5 – 85.0], p = .039). In the analysis for ICU admission, significant predictors were diverticular perforation (OR = 11.1, 95% CI: 3.9 – 31.9], p < .001), NAFLD (OR = 5.7, 95% CI: 1.4 – 22.6], p = .014), and alcohol use (OR = 3.9, 95% CI: 1.5 – 10.1], p = .005). Surgery (p < .001) and colonoscopies (p = .002) were associated with increased LOS.
Discussion: In this retrospective study, we discovered that admission for diverticular bleeding and history of NAFLD were associated with increased mortality. NAFLD, perforation, and alcohol use increased the risk for ICU stay, while longer LOS was seen for patients who underwent surgery or colonoscopy.
Disclosures:
Kevin Yang indicated no relevant financial relationships.
Gregory Gudleski indicated no relevant financial relationships.
Ali Aijaz indicated no relevant financial relationships.
Omar Arman indicated no relevant financial relationships.
Corrine Kickel indicated no relevant financial relationships.
Nariman Hossein-Javaheri indicated no relevant financial relationships.
Alexander Carlson indicated no relevant financial relationships.
Matthew Hudson indicated no relevant financial relationships.
Mayada Ismail indicated no relevant financial relationships.
Kevin Yang, MD, Gregory D. Gudleski, PhD, Ali A.. Aijaz, DO, Omar Arman, MD, Corrine Kickel, MD, Nariman Hossein-Javaheri, DO, Alexander M. Carlson, DO, Matthew J.. Hudson, MD, Mayada Ismail, MD. P3005 - Predictors of Outcomes in Hospitalization for Diverticular Disease, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
