Tuesday Poster Session
Category: Liver
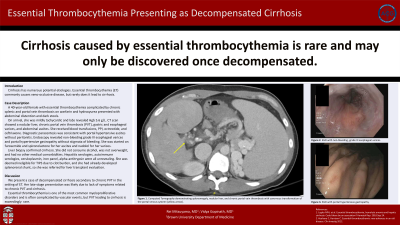
P4008 - Essential Thrombocythemia Presenting as Decompensated Cirrhosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
Rei Mitsuyama, MD
Brown University
Providence, RI
Presenting Author(s)
Rei Mitsuyama, MD, Vidya Goipinath, MD
Brown University, Providence, RI
Introduction: Cirrhosis represents late stage hepatic fibrosis with numerous potential etiologies. Though veno-occlusive disease is a common manifestation of essential thrombocythemia (ET), it is rarely implicated as a cause of cirrhosis.
Case Description/Methods: A 40-year-old female with past medical history of essential thrombocythemia complicated by chronic splenic and portal vein thrombosis on warfarin and hydroxyurea presented with abdominal distention and dark stools. She also endorsed fatigue, decreased appetite, and lightheadedness.
On arrival, she was tachycardic to the 100s but normotensive. Labs revealed Hgb 5.6 g/L. CT scan demonstrated a nodular liver, chronic portal vein thrombosis, gastric and esophageal varices, and abdominal ascites. She was transfused 3 units of packed red blood cells and started on a PPI, octreotide, and ceftriaxone. Diagnostic paracentesis was consistent with portal hypertensive ascites without peritonitis. Endoscopy revealed non-bleeding grade III esophageal varices and portal hypertensive gastropathy without stigmata of bleeding. She was started on furosemide and spironolactone for her ascites and nadolol for her varices.
Liver biopsy confirmed cirrhosis, the etiology of which was thought to be chronic portal vein thrombosis. The patient did not consume alcohol, was not overweight, and had no other medical comorbidities. Hepatitis serologies, autoimmune serologies, ceruloplasmin, iron panel, alpha-antitrypsin were all unrevealing of an alternate etiology. She was deemed ineligible for TIPS due to clot burden, and she had already developed splenorenal shunt, so she was referred for liver transplant evaluation.
Discussion: We present a case of decompensated cirrhosis secondary to chronic portal vein thrombosis in the setting of essential thrombocythemia. This unfortunately late-stage presentation is perhaps unsurprising given chronic PVT and cirrhosis can be asymptomatic early on. There have been few reported cases of cirrhosis caused by ET. In all cases, patients had known diagnosis of ET and were only discovered to have cirrhosis once they presented with ascites.
Essential thrombocythemia is one of the most common myeloproliferative disorders and is often complicated by vascular events. Headaches, dizziness, strokes, and splenomegaly are more commonly reported symptoms of vaso-occlusion, but many patients have no symptoms at the time of diagnosis. A case could be made to screen patients for cirrhosis who have known ET, particularly if they have developed PVT.

Disclosures:
Rei Mitsuyama, MD, Vidya Goipinath, MD. P4008 - Essential Thrombocythemia Presenting as Decompensated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
Brown University, Providence, RI
Introduction: Cirrhosis represents late stage hepatic fibrosis with numerous potential etiologies. Though veno-occlusive disease is a common manifestation of essential thrombocythemia (ET), it is rarely implicated as a cause of cirrhosis.
Case Description/Methods: A 40-year-old female with past medical history of essential thrombocythemia complicated by chronic splenic and portal vein thrombosis on warfarin and hydroxyurea presented with abdominal distention and dark stools. She also endorsed fatigue, decreased appetite, and lightheadedness.
On arrival, she was tachycardic to the 100s but normotensive. Labs revealed Hgb 5.6 g/L. CT scan demonstrated a nodular liver, chronic portal vein thrombosis, gastric and esophageal varices, and abdominal ascites. She was transfused 3 units of packed red blood cells and started on a PPI, octreotide, and ceftriaxone. Diagnostic paracentesis was consistent with portal hypertensive ascites without peritonitis. Endoscopy revealed non-bleeding grade III esophageal varices and portal hypertensive gastropathy without stigmata of bleeding. She was started on furosemide and spironolactone for her ascites and nadolol for her varices.
Liver biopsy confirmed cirrhosis, the etiology of which was thought to be chronic portal vein thrombosis. The patient did not consume alcohol, was not overweight, and had no other medical comorbidities. Hepatitis serologies, autoimmune serologies, ceruloplasmin, iron panel, alpha-antitrypsin were all unrevealing of an alternate etiology. She was deemed ineligible for TIPS due to clot burden, and she had already developed splenorenal shunt, so she was referred for liver transplant evaluation.
Discussion: We present a case of decompensated cirrhosis secondary to chronic portal vein thrombosis in the setting of essential thrombocythemia. This unfortunately late-stage presentation is perhaps unsurprising given chronic PVT and cirrhosis can be asymptomatic early on. There have been few reported cases of cirrhosis caused by ET. In all cases, patients had known diagnosis of ET and were only discovered to have cirrhosis once they presented with ascites.
Essential thrombocythemia is one of the most common myeloproliferative disorders and is often complicated by vascular events. Headaches, dizziness, strokes, and splenomegaly are more commonly reported symptoms of vaso-occlusion, but many patients have no symptoms at the time of diagnosis. A case could be made to screen patients for cirrhosis who have known ET, particularly if they have developed PVT.

Figure: Figure 1. A - CT demonstrating nodular liver and chronic portal vein thrombosis with cavernous transformation. B - EGD with non-bleeding, grade III esophageal varices. C - EGD with portal hypertensive gastropathy.
Disclosures:
Rei Mitsuyama indicated no relevant financial relationships.
Vidya Goipinath indicated no relevant financial relationships.
Rei Mitsuyama, MD, Vidya Goipinath, MD. P4008 - Essential Thrombocythemia Presenting as Decompensated Cirrhosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
