Tuesday Poster Session
Category: Liver
P4010 - Hepatic Tuberculosis With Concomitant Pulmonary Tuberculosis
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio
- MA
Mohammad Jamal Abushanab, MD
Saint Michael's Medical Center
Newark, New Jersey
Presenting Author(s)
Mohammad Jamal Abushanab, MD1, Ayushi Mohan, MD1, Saraswathi Lakkasani, MD2, Muhammad Hussain, MD2, Byron Okwesili, MD2, Jihad Slim, MD1, Mehul Shah, MD1
1Saint Michael's Medical Center, Newark, NJ; 2Saint Michael's Medical Center, New York Medical College, Newark, NJ
Introduction: Tuberculosis (TB) is a systemic chronic infectious disease mainly affects the lungs. Hepatic tuberculosis is relatively rare and often misdiagnosed. Here we are reporting a Case of Pulmonary TB with concomitant Hepatic TB.
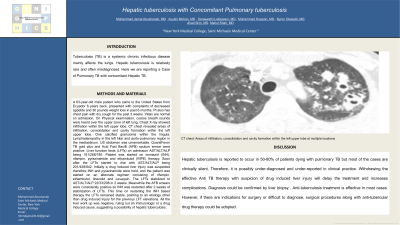
Case Description/Methods: A 63-year-old male patient who came to the United States from Ecuador 6 years back, presented with complaints of decreased appetite and 30 pounds weight loss in past 6 months. Pt also has chest pain with dry cough for the past 3 weeks. Vitals are normal on admission. On Physical examination, coarse breath sounds were heard over the upper zone of left lung. Chest X-ray showed infiltration within the left upper lobe. CT chest revealed areas of infiltration, consolidation and cavity formation within the left upper lobe. One calcified granuloma within the lingula. Lymphadenopathy in the left hilar and aorto-pulmonary region in the mediastinum. US abdomen was unremarkable. QuantiFeron TB gold plus and Acid Fast Bacilli (AFB) sputum smear were positive. Liver function tests (LFTs) on admission AST/ALT/ALP being 161/268/180. Patient was started on isoniazid (INH), rifampin, pyrazinamide and ethambutol (RIPE) therapy. Soon after the LFTs started to rise with AST/ALT/ALP being 201/428/842. Initially a drug induced liver injury was suspected therefore INH and pyrazinamide were held, and the patient was started on an alternate regimen consisting of rifampin, ethambutol, linezolid and Levaquin. The LFTs stabilized to AST/ALT/ALP 22/33/208 in 2 weeks. Meanwhile the AFB smears were consistently positive so INH was restarted after 2 weeks of stabilization of LFTs. This time on restarting the INH based therapy the LFTs remained stable, pointing to an etiology other than drug induced injury for the previous LFT elevations. All the liver work up was negative, ruling out an immunologic or a drug induced cause, suggesting a possibility of hepatic tuberculosis.
Discussion: Hepatic tuberculosis is reported to occur in 50-80% of patients dying with pulmonary TB but most of the cases are clinically silent. Therefore, it is possibly under-diagnosed and under-reported in clinical practice. Withdrawing the effective Anti TB therapy with suspicion of drug induced liver injury will delay the treatment and increases complications. Diagnosis could be confirmed by liver biopsy . Anti-tuberculosis treatment is effective in most cases. However, if there are indications for surgery or difficult to diagnose, surgical procedures along with anti-tubercular drug therapy could be adopted.

Disclosures:
Mohammad Jamal Abushanab, MD1, Ayushi Mohan, MD1, Saraswathi Lakkasani, MD2, Muhammad Hussain, MD2, Byron Okwesili, MD2, Jihad Slim, MD1, Mehul Shah, MD1. P4010 - Hepatic Tuberculosis With Concomitant Pulmonary Tuberculosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Saint Michael's Medical Center, Newark, NJ; 2Saint Michael's Medical Center, New York Medical College, Newark, NJ
Introduction: Tuberculosis (TB) is a systemic chronic infectious disease mainly affects the lungs. Hepatic tuberculosis is relatively rare and often misdiagnosed. Here we are reporting a Case of Pulmonary TB with concomitant Hepatic TB.
Case Description/Methods: A 63-year-old male patient who came to the United States from Ecuador 6 years back, presented with complaints of decreased appetite and 30 pounds weight loss in past 6 months. Pt also has chest pain with dry cough for the past 3 weeks. Vitals are normal on admission. On Physical examination, coarse breath sounds were heard over the upper zone of left lung. Chest X-ray showed infiltration within the left upper lobe. CT chest revealed areas of infiltration, consolidation and cavity formation within the left upper lobe. One calcified granuloma within the lingula. Lymphadenopathy in the left hilar and aorto-pulmonary region in the mediastinum. US abdomen was unremarkable. QuantiFeron TB gold plus and Acid Fast Bacilli (AFB) sputum smear were positive. Liver function tests (LFTs) on admission AST/ALT/ALP being 161/268/180. Patient was started on isoniazid (INH), rifampin, pyrazinamide and ethambutol (RIPE) therapy. Soon after the LFTs started to rise with AST/ALT/ALP being 201/428/842. Initially a drug induced liver injury was suspected therefore INH and pyrazinamide were held, and the patient was started on an alternate regimen consisting of rifampin, ethambutol, linezolid and Levaquin. The LFTs stabilized to AST/ALT/ALP 22/33/208 in 2 weeks. Meanwhile the AFB smears were consistently positive so INH was restarted after 2 weeks of stabilization of LFTs. This time on restarting the INH based therapy the LFTs remained stable, pointing to an etiology other than drug induced injury for the previous LFT elevations. All the liver work up was negative, ruling out an immunologic or a drug induced cause, suggesting a possibility of hepatic tuberculosis.
Discussion: Hepatic tuberculosis is reported to occur in 50-80% of patients dying with pulmonary TB but most of the cases are clinically silent. Therefore, it is possibly under-diagnosed and under-reported in clinical practice. Withdrawing the effective Anti TB therapy with suspicion of drug induced liver injury will delay the treatment and increases complications. Diagnosis could be confirmed by liver biopsy . Anti-tuberculosis treatment is effective in most cases. However, if there are indications for surgery or difficult to diagnose, surgical procedures along with anti-tubercular drug therapy could be adopted.

Figure: CT chest: Areas of infiltration, consolidation and cavity formation within the left upper lobe at multiple locations
Disclosures:
Mohammad Jamal Abushanab indicated no relevant financial relationships.
Ayushi Mohan indicated no relevant financial relationships.
Saraswathi Lakkasani indicated no relevant financial relationships.
Muhammad Hussain indicated no relevant financial relationships.
Byron Okwesili indicated no relevant financial relationships.
Jihad Slim indicated no relevant financial relationships.
Mehul Shah indicated no relevant financial relationships.
Mohammad Jamal Abushanab, MD1, Ayushi Mohan, MD1, Saraswathi Lakkasani, MD2, Muhammad Hussain, MD2, Byron Okwesili, MD2, Jihad Slim, MD1, Mehul Shah, MD1. P4010 - Hepatic Tuberculosis With Concomitant Pulmonary Tuberculosis, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
