Tuesday Poster Session
Category: Liver
P3894 - A Case of Late-Onset Hepatic Sinusoidal Obstructive Syndrome/Veno-Occlusive Disease One Year Post Transplant
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Mary White, MD
Yale New Haven Hospital
New Haven, CT
Presenting Author(s)
Mary White, MD1, Meagan Alvarado, MD2, Albina Joldoshova, MD1, Xuchen Zhang, MD, PhD1, Bubu Banini, MD, PhD3
1Yale New Haven Hospital, New Haven, CT; 2Yale University School of Medicine, New Haven, CT; 3Yale School of Medicine, New Haven, CT
Introduction: Sinusoidal obstructive syndrome (SOS), also known as veno-occlusive disease, is a clinical syndrome characterized by systemic endothelial injury that typically develops within 21 days after hematopoietic cell transplantation. Rare cases occurring after 21 days are termed late-onset SOS. Injury occurring in SOS is thought to be due to chemotherapy metabolites that damage hepatic sinusoidal epithelial cells leading to venous outflow obstruction and post-sinusoidal portal hypertension. Mortality for severe SOS exceeds 80%. Here, we report SOS occurring 350 days after transplant, which to our knowledge illustrates the longest period of latency prior to SOS onset that has been reported in the literature.
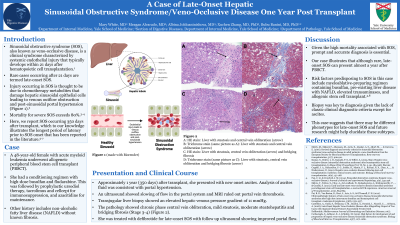
Case Description/Methods: A 48-year-old female with acute myeloid leukemia underwent allogeneic peripheral blood stem cell transplant (PBSCT) after a conditioning regimen with high-dose busulfan and fludarabine, followed by prophylactic ursodiol therapy, tacrolimus and cellcept for immunosuppression, and azacitidine for maintenance. Other history includes non-alcoholic fatty liver disease (NAFLD) without known fibrosis. Approximately 1 year (350 days) after transplant, she presented with new onset ascites. Analysis of ascites fluid was consistent with portal hypertension. An ultrasound showed slowing of flow in the portal system and MRI ruled out portal vein thrombosis. Transjugular liver biopsy showed elevated hepatic venous pressure gradient of 11 mmHg, chronic phase central vein obliteration, mild steatosis, moderate steatohepatitis and bridging fibrosis (Stage 3-4) (Images 1-3). She was treated with defibrotide for late-onset SOS with follow up ultrasound showing improved portal flow.
Discussion: Given the high mortality associated with SOS, prompt and accurate diagnosis is essential. Our case illustrates that although rare, late-onset SOS can present almost a year after PBSCT. Risk factors predisposing to SOS in this case include myeloablative-preparing regimen containing busulfan, pre-existing liver disease with NAFLD, elevated transaminases, and allogenic stem cell transplant. Biopsy was key to diagnosis given the lack of classic clinical diagnostic criteria except for ascites. This case suggests that there may be different phenotypes for late-onset SOS and future research might help elucidate these subtypes.

Disclosures:
Mary White, MD1, Meagan Alvarado, MD2, Albina Joldoshova, MD1, Xuchen Zhang, MD, PhD1, Bubu Banini, MD, PhD3. P3894 - A Case of Late-Onset Hepatic Sinusoidal Obstructive Syndrome/Veno-Occlusive Disease One Year Post Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Yale New Haven Hospital, New Haven, CT; 2Yale University School of Medicine, New Haven, CT; 3Yale School of Medicine, New Haven, CT
Introduction: Sinusoidal obstructive syndrome (SOS), also known as veno-occlusive disease, is a clinical syndrome characterized by systemic endothelial injury that typically develops within 21 days after hematopoietic cell transplantation. Rare cases occurring after 21 days are termed late-onset SOS. Injury occurring in SOS is thought to be due to chemotherapy metabolites that damage hepatic sinusoidal epithelial cells leading to venous outflow obstruction and post-sinusoidal portal hypertension. Mortality for severe SOS exceeds 80%. Here, we report SOS occurring 350 days after transplant, which to our knowledge illustrates the longest period of latency prior to SOS onset that has been reported in the literature.
Case Description/Methods: A 48-year-old female with acute myeloid leukemia underwent allogeneic peripheral blood stem cell transplant (PBSCT) after a conditioning regimen with high-dose busulfan and fludarabine, followed by prophylactic ursodiol therapy, tacrolimus and cellcept for immunosuppression, and azacitidine for maintenance. Other history includes non-alcoholic fatty liver disease (NAFLD) without known fibrosis. Approximately 1 year (350 days) after transplant, she presented with new onset ascites. Analysis of ascites fluid was consistent with portal hypertension. An ultrasound showed slowing of flow in the portal system and MRI ruled out portal vein thrombosis. Transjugular liver biopsy showed elevated hepatic venous pressure gradient of 11 mmHg, chronic phase central vein obliteration, mild steatosis, moderate steatohepatitis and bridging fibrosis (Stage 3-4) (Images 1-3). She was treated with defibrotide for late-onset SOS with follow up ultrasound showing improved portal flow.
Discussion: Given the high mortality associated with SOS, prompt and accurate diagnosis is essential. Our case illustrates that although rare, late-onset SOS can present almost a year after PBSCT. Risk factors predisposing to SOS in this case include myeloablative-preparing regimen containing busulfan, pre-existing liver disease with NAFLD, elevated transaminases, and allogenic stem cell transplant. Biopsy was key to diagnosis given the lack of classic clinical diagnostic criteria except for ascites. This case suggests that there may be different phenotypes for late-onset SOS and future research might help elucidate these subtypes.

Figure: Image 1: Central vein obliteration with bridging fibrosis
Image 2: Central vein dense fibrosis and obliteration - bottom right of image
Image 3: Central vein obliteration with centrilobular drop out on Trichrome stain
Image 2: Central vein dense fibrosis and obliteration - bottom right of image
Image 3: Central vein obliteration with centrilobular drop out on Trichrome stain
Disclosures:
Mary White indicated no relevant financial relationships.
Meagan Alvarado indicated no relevant financial relationships.
Albina Joldoshova indicated no relevant financial relationships.
Xuchen Zhang indicated no relevant financial relationships.
Bubu Banini indicated no relevant financial relationships.
Mary White, MD1, Meagan Alvarado, MD2, Albina Joldoshova, MD1, Xuchen Zhang, MD, PhD1, Bubu Banini, MD, PhD3. P3894 - A Case of Late-Onset Hepatic Sinusoidal Obstructive Syndrome/Veno-Occlusive Disease One Year Post Transplant, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
