Tuesday Poster Session
Category: Biliary/Pancreas
P2894 - The Great Mimicker: A Case Series of Autoimmune Pancreatitis Initially Presenting as a Pancreatic Mass Concerning for Malignancy
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Brian Lee, DO
Texas Tech University Health Sciences Center
El Paso, TX
Presenting Author(s)
Brian Lee, DO1, Swati Mahapatra, DO2, Jesus Guzman, MD3, Ioannis Konstantinidis, MD1, Vital Rangashamanna, MD4, Nawar Hakim, MD1, Sherif E. Elhanafi, MD1
1Texas Tech University Health Sciences Center, El Paso, TX; 2Texas Tech University of Health Sciences, El Paso, TX; 3Texas Tech Health Science Center, El Paso, TX; 4Texas Tech, El Paso, TX
Introduction: Autoimmune pancreatitis (AIP) is a rare form of pancreatitis that is diagnosed based on clinical, radiographic, serological, and biopsy findings. It is characterized by swelling of the pancreas and narrowing of the pancreatic duct due to an abnormal immune response. Diagnosis is challenging as AIP can present as a pancreatic mass, and thus must be differentiated from pancreatic malignancy. Distinguishing these entities is crucial as there are differences in treatment course and prognosis. Herein, we present a case series of four patients that presented with a mass concerning for pancreatic cancer, with subsequent work up confirming the diagnosis of AIP.
Case Description/Methods: Our patients include three males (32, 55, and 68 years) and one female (73 years). These patients presented with abdominal pain (n=2), scleral icterus (n=3), and pruritus (n=1). All four of the patients had elevated total and direct bilirubin, and further work up revealed elevated serum IgG4. One patient had a mildly elevated CA 19-9 of 76 U/mL (normal < 34). All patients underwent a contrast-enhanced computed tomography (CT) or magnetic resonance of the abdomen that identified a pancreatic mass. All patients underwent endoscopic ultrasound (EUS) with fine needle biopsy (FNB). Findings from FNB were negative for malignancy in all patients. Three of the biopsies exhibited negative IgG4 and CD138 staining. Biopsy results noted normal pancreatic acinar cells for all patients, as well as chronic inflammation and fibrosis in three patients. ERCP was performed for all patients as well, with stent placement for biliary decompression. All patients had follow-up ERCP with subsequent stent removal and no recurrence of biliary obstruction over the follow-up period. Once the diagnosis of AIP was validated, each patient was started on a steroid taper course, which resulted in improvement of patients’ symptoms and complete resolution of radiological evidence of pancreatic mass, confirming the diagnosis of AIP. The patients remained symptom-free with no signs of relapse at 3, 6, and 12-month follow ups.
Discussion: This case series highlights the similarities between pancreatic cancer and AIP. A full work up including cross sectional imaging and EUS with FNB should be considered before entertaining the diagnosis of AIP.

Disclosures:
Brian Lee, DO1, Swati Mahapatra, DO2, Jesus Guzman, MD3, Ioannis Konstantinidis, MD1, Vital Rangashamanna, MD4, Nawar Hakim, MD1, Sherif E. Elhanafi, MD1. P2894 - The Great Mimicker: A Case Series of Autoimmune Pancreatitis Initially Presenting as a Pancreatic Mass Concerning for Malignancy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Texas Tech University Health Sciences Center, El Paso, TX; 2Texas Tech University of Health Sciences, El Paso, TX; 3Texas Tech Health Science Center, El Paso, TX; 4Texas Tech, El Paso, TX
Introduction: Autoimmune pancreatitis (AIP) is a rare form of pancreatitis that is diagnosed based on clinical, radiographic, serological, and biopsy findings. It is characterized by swelling of the pancreas and narrowing of the pancreatic duct due to an abnormal immune response. Diagnosis is challenging as AIP can present as a pancreatic mass, and thus must be differentiated from pancreatic malignancy. Distinguishing these entities is crucial as there are differences in treatment course and prognosis. Herein, we present a case series of four patients that presented with a mass concerning for pancreatic cancer, with subsequent work up confirming the diagnosis of AIP.
Case Description/Methods: Our patients include three males (32, 55, and 68 years) and one female (73 years). These patients presented with abdominal pain (n=2), scleral icterus (n=3), and pruritus (n=1). All four of the patients had elevated total and direct bilirubin, and further work up revealed elevated serum IgG4. One patient had a mildly elevated CA 19-9 of 76 U/mL (normal < 34). All patients underwent a contrast-enhanced computed tomography (CT) or magnetic resonance of the abdomen that identified a pancreatic mass. All patients underwent endoscopic ultrasound (EUS) with fine needle biopsy (FNB). Findings from FNB were negative for malignancy in all patients. Three of the biopsies exhibited negative IgG4 and CD138 staining. Biopsy results noted normal pancreatic acinar cells for all patients, as well as chronic inflammation and fibrosis in three patients. ERCP was performed for all patients as well, with stent placement for biliary decompression. All patients had follow-up ERCP with subsequent stent removal and no recurrence of biliary obstruction over the follow-up period. Once the diagnosis of AIP was validated, each patient was started on a steroid taper course, which resulted in improvement of patients’ symptoms and complete resolution of radiological evidence of pancreatic mass, confirming the diagnosis of AIP. The patients remained symptom-free with no signs of relapse at 3, 6, and 12-month follow ups.
Discussion: This case series highlights the similarities between pancreatic cancer and AIP. A full work up including cross sectional imaging and EUS with FNB should be considered before entertaining the diagnosis of AIP.

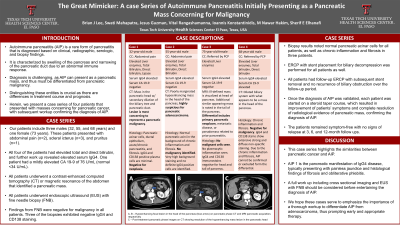
Figure: A, B – Hypoenhancing focal lesion in the head of pancreas (blue arrow) on pancreatic phase CT and MRI pancreatic acquisition, respectively
C – Post-treatment pancreatic phase images on CT showing resolution of the hypoenhancing mass lesion in the pancreatic head
C – Post-treatment pancreatic phase images on CT showing resolution of the hypoenhancing mass lesion in the pancreatic head
Disclosures:
Brian Lee indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Jesus Guzman indicated no relevant financial relationships.
Ioannis Konstantinidis indicated no relevant financial relationships.
Vital Rangashamanna indicated no relevant financial relationships.
Nawar Hakim indicated no relevant financial relationships.
Sherif Elhanafi indicated no relevant financial relationships.
Brian Lee, DO1, Swati Mahapatra, DO2, Jesus Guzman, MD3, Ioannis Konstantinidis, MD1, Vital Rangashamanna, MD4, Nawar Hakim, MD1, Sherif E. Elhanafi, MD1. P2894 - The Great Mimicker: A Case Series of Autoimmune Pancreatitis Initially Presenting as a Pancreatic Mass Concerning for Malignancy, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
