Tuesday Poster Session
Category: Biliary/Pancreas
P2897 - Hemorrhagic Pancreatic Ascites Treated With Pancreatic Duct Stenting
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Gina Moon, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Gina Moon, MD1, Jalal Gondal, BA2, Omar Amayem, DO3, Tokunbo Ajayi, MD2, William M. Tierney, MD1
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK; 3HCA Healthcare Mid-America Division, Kansas City, MO
Introduction: Ascites is typically caused by chronic liver disease (80%), malignancy (10%), and congestive heart failure (3-5%). Rare causes include pancreatic, biliary, infectious, and others, each representing less than 1% of cases. Pancreatic ascites is secondary to continuous pancreatic secretion trickling into the peritoneum due to anterior pancreatic ductal disruption, secondary to leakage of a ruptured pseudocyst into the duct. Posterior ductal disruption causes pleural effusions. Ascitic fluid studies will reveal total protein > 3g/dL, amylase > 1,000u/l, and SAAG < 1.1. This case is unique as our patient presented with hemorrhagic ascites which was responsive to pancreatic duct stenting alone.
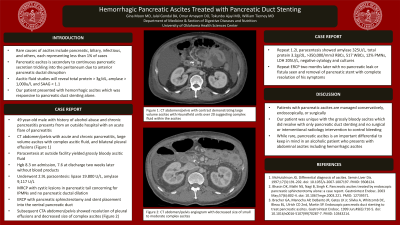
Case Description/Methods: A 49 year-old male with history of alcohol abuse and chronic pancreatitis presents from an outside hospital with an acute flare of pancreatitis. He endorsed diffuse, crampy abdominal pain with distension. CT abdomen/pelvis with acute and chronic pancreatitis, large volume ascites with complex ascitic fluid, and bilateral pleural effusions (Image1). Paracentesis at the outside facility yielded grossly bloody ascitic fluid and he was transferred to our center to manage the hemorrhagic ascites. His hemoglobin on admission was 8.3, then 7.6 at discharge two weeks later without any blood product transfusions. He underwent a 2.9L paracentesis notable for lipase 19,800U/L, amylase 9,117U/L. MRCP with cystic lesions in pancreatic tail concerning for IPMNs and no pancreatic ductal dilation. He underwent an ERCP with pancreatic sphincterotomy and stent placement into the ventral pancreatic duct. Subsequent CTA abdomen/pelvis showed resolution of pleural effusions and decreased size of complex ascites (Image1). A repeat 1.2L paracentesis showed amylase 325U/L, total protein 3.2g/dL, >350,000/mm3 RBCs, 517 WBCs, 12% PMNs, LDH 205U/L, negative cytology and cultures. He underwent a repeat ERCP two months later with no pancreatic leak or fistula seen and removal of pancreatic stent with complete resolution of his symptoms (Image1).
Discussion: Patients with pancreatic ascites are managed conservatively, endoscopically, or surgically. Our patient was unique with the grossly bloody ascites which did resolve with only pancreatic duct stenting and no surgical or interventional radiology intervention to control bleeding. While rare, pancreatic ascites is an important differential to keep in mind in an alcoholic patient who presents with abdominal ascites including hemorrhagic ascites.

Disclosures:
Gina Moon, MD1, Jalal Gondal, BA2, Omar Amayem, DO3, Tokunbo Ajayi, MD2, William M. Tierney, MD1. P2897 - Hemorrhagic Pancreatic Ascites Treated With Pancreatic Duct Stenting, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2University of Oklahoma College of Medicine, Oklahoma City, OK; 3HCA Healthcare Mid-America Division, Kansas City, MO
Introduction: Ascites is typically caused by chronic liver disease (80%), malignancy (10%), and congestive heart failure (3-5%). Rare causes include pancreatic, biliary, infectious, and others, each representing less than 1% of cases. Pancreatic ascites is secondary to continuous pancreatic secretion trickling into the peritoneum due to anterior pancreatic ductal disruption, secondary to leakage of a ruptured pseudocyst into the duct. Posterior ductal disruption causes pleural effusions. Ascitic fluid studies will reveal total protein > 3g/dL, amylase > 1,000u/l, and SAAG < 1.1. This case is unique as our patient presented with hemorrhagic ascites which was responsive to pancreatic duct stenting alone.
Case Description/Methods: A 49 year-old male with history of alcohol abuse and chronic pancreatitis presents from an outside hospital with an acute flare of pancreatitis. He endorsed diffuse, crampy abdominal pain with distension. CT abdomen/pelvis with acute and chronic pancreatitis, large volume ascites with complex ascitic fluid, and bilateral pleural effusions (Image1). Paracentesis at the outside facility yielded grossly bloody ascitic fluid and he was transferred to our center to manage the hemorrhagic ascites. His hemoglobin on admission was 8.3, then 7.6 at discharge two weeks later without any blood product transfusions. He underwent a 2.9L paracentesis notable for lipase 19,800U/L, amylase 9,117U/L. MRCP with cystic lesions in pancreatic tail concerning for IPMNs and no pancreatic ductal dilation. He underwent an ERCP with pancreatic sphincterotomy and stent placement into the ventral pancreatic duct. Subsequent CTA abdomen/pelvis showed resolution of pleural effusions and decreased size of complex ascites (Image1). A repeat 1.2L paracentesis showed amylase 325U/L, total protein 3.2g/dL, >350,000/mm3 RBCs, 517 WBCs, 12% PMNs, LDH 205U/L, negative cytology and cultures. He underwent a repeat ERCP two months later with no pancreatic leak or fistula seen and removal of pancreatic stent with complete resolution of his symptoms (Image1).
Discussion: Patients with pancreatic ascites are managed conservatively, endoscopically, or surgically. Our patient was unique with the grossly bloody ascites which did resolve with only pancreatic duct stenting and no surgical or interventional radiology intervention to control bleeding. While rare, pancreatic ascites is an important differential to keep in mind in an alcoholic patient who presents with abdominal ascites including hemorrhagic ascites.

Figure: Image 1: Panel A - CT abdomen/pelvis with contrast demonstrating large volume ascites with Hounsfield units over 20 suggesting complex fluid within the ascites. Panel B - CT abdomen/pelvis angiogram with decreased size of small to moderate complex ascites. Panel C - ERCP with IV contrast demonstrating patency of the ventral pancreatic stent.
Disclosures:
Gina Moon indicated no relevant financial relationships.
Jalal Gondal indicated no relevant financial relationships.
Omar Amayem indicated no relevant financial relationships.
Tokunbo Ajayi indicated no relevant financial relationships.
William Tierney indicated no relevant financial relationships.
Gina Moon, MD1, Jalal Gondal, BA2, Omar Amayem, DO3, Tokunbo Ajayi, MD2, William M. Tierney, MD1. P2897 - Hemorrhagic Pancreatic Ascites Treated With Pancreatic Duct Stenting, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
