Tuesday Poster Session
Category: Biliary/Pancreas
P2899 - A Pseudoaneurysm Within a Pancreatic Pseudocyst: A Rare Complication Managed With Endovascular Stenting
Tuesday, October 24, 2023
10:30 AM - 4:00 PM PT
Location: Exhibit Hall
Has Audio

Nigil Thaimuriyil, DO
Baptist Hospitals of Southeast Texas
Beaumont, TX
Presenting Author(s)
Amr Hamed, MD1, Nigil Thaimuriyil, DO2, Ahmed Abdelhakeem, MD1, Mohamed Vadva, MD3, Robert Morrison, MD4
1Baptist Hospitals of Southeast Texas, Beaumont, TX; 2Baptist Hospitals of Southeast Texas, Newark, NJ; 3Baptist Physicians Network, Beaumont, TX; 4Coastal Imaging Associates, Beaumont, TX
Introduction: Pancreatic pseudocysts are a common complication of chronic pancreatitis. Rarely, chronic pancreatitis can cause excessive release of pancreatic enzymes that digest elastin fibers in arterial walls, destroying arterial architecture and forming a pseudoaneurysm. We present a case of a pancreatic pseudocyst complicated by a pseudoaneurysm of the splenic artery, successfully managed by endovascular stenting at a community hospital.
Case Description/Methods: A 67-year-old male with a history of chronic pancreatitis presented to the emergency room (ER) with nausea and epigastric pain. Eight days prior, he underwent Endoscopic Ultrasound with Fine Needle Aspiration (EUS-FNA) to evaluate a cystic structure in the body of the pancreas. Cytology from the aspirant showed a CEA level of 39 and an amylase of 28,644, consistent with a pancreatic pseudocyst. In the ER, CT scan abdomen with contrast revealed acute pancreatitis and a 2.5 cm pseudoaneurysm within the body of the pancreas, arising from the splenic artery, and solid and cystic pancreatic head lesions with evidence of internal hemorrhage. Lipase level was 3351. Aggressive fluid resuscitation and opioid analgesics were initiated. Three days later, patient underwent successful CT-guided endovascular stent grafting of the splenic artery. Patient was seen in the GI clinic with complete resolution of acute symptoms.
Discussion: Severe chronic pancreatitis can produce enzymes that digest the elastin fibers of arteries leading to distortion of the arterial wall architecture and formation of pseudoaneurysms. Pancreatic pseudoaneurysms are most common in the splenic artery. We suspect that the pseudocyst leaked digestive enzymes into the surrounding area, predisposing the vasculature to damage during the recent EUS-FNA and internal hemorrhage within the pancreas. A pancreatic pseudoaneurysm should be treated regardless of its size, as it carries an elevated risk of rupture and mortality if left untreated. Common modalities used to treat them include endovascular coiling, stenting, and rarely, surgical resection. In this patient's case in our community hospital, the interventionalist opted to employ a covered stent using an endovascular approach, which he was most familiar with. Here we highlight one of the dangerous complications of pancreatitis that requires prompt recognition and intervention to avoid hemorrhage and mortality. These patients should be monitored closely as the risk for hemorrhage remains high following intervention.

Disclosures:
Amr Hamed, MD1, Nigil Thaimuriyil, DO2, Ahmed Abdelhakeem, MD1, Mohamed Vadva, MD3, Robert Morrison, MD4. P2899 - A Pseudoaneurysm Within a Pancreatic Pseudocyst: A Rare Complication Managed With Endovascular Stenting, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
1Baptist Hospitals of Southeast Texas, Beaumont, TX; 2Baptist Hospitals of Southeast Texas, Newark, NJ; 3Baptist Physicians Network, Beaumont, TX; 4Coastal Imaging Associates, Beaumont, TX
Introduction: Pancreatic pseudocysts are a common complication of chronic pancreatitis. Rarely, chronic pancreatitis can cause excessive release of pancreatic enzymes that digest elastin fibers in arterial walls, destroying arterial architecture and forming a pseudoaneurysm. We present a case of a pancreatic pseudocyst complicated by a pseudoaneurysm of the splenic artery, successfully managed by endovascular stenting at a community hospital.
Case Description/Methods: A 67-year-old male with a history of chronic pancreatitis presented to the emergency room (ER) with nausea and epigastric pain. Eight days prior, he underwent Endoscopic Ultrasound with Fine Needle Aspiration (EUS-FNA) to evaluate a cystic structure in the body of the pancreas. Cytology from the aspirant showed a CEA level of 39 and an amylase of 28,644, consistent with a pancreatic pseudocyst. In the ER, CT scan abdomen with contrast revealed acute pancreatitis and a 2.5 cm pseudoaneurysm within the body of the pancreas, arising from the splenic artery, and solid and cystic pancreatic head lesions with evidence of internal hemorrhage. Lipase level was 3351. Aggressive fluid resuscitation and opioid analgesics were initiated. Three days later, patient underwent successful CT-guided endovascular stent grafting of the splenic artery. Patient was seen in the GI clinic with complete resolution of acute symptoms.
Discussion: Severe chronic pancreatitis can produce enzymes that digest the elastin fibers of arteries leading to distortion of the arterial wall architecture and formation of pseudoaneurysms. Pancreatic pseudoaneurysms are most common in the splenic artery. We suspect that the pseudocyst leaked digestive enzymes into the surrounding area, predisposing the vasculature to damage during the recent EUS-FNA and internal hemorrhage within the pancreas. A pancreatic pseudoaneurysm should be treated regardless of its size, as it carries an elevated risk of rupture and mortality if left untreated. Common modalities used to treat them include endovascular coiling, stenting, and rarely, surgical resection. In this patient's case in our community hospital, the interventionalist opted to employ a covered stent using an endovascular approach, which he was most familiar with. Here we highlight one of the dangerous complications of pancreatitis that requires prompt recognition and intervention to avoid hemorrhage and mortality. These patients should be monitored closely as the risk for hemorrhage remains high following intervention.

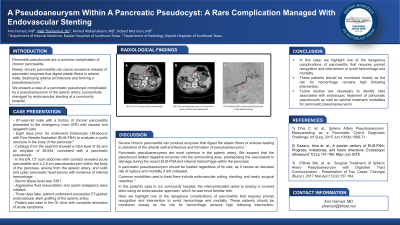
Figure: (A) 2.8 x 2.7cm pancreatic pseudocyst
(B) 2.5cm pseudoaneurysm of the splenic artery within the pseudocyst
(C) Covered stent endoscopically placed in the splenic artery
(B) 2.5cm pseudoaneurysm of the splenic artery within the pseudocyst
(C) Covered stent endoscopically placed in the splenic artery
Disclosures:
Amr Hamed indicated no relevant financial relationships.
Nigil Thaimuriyil indicated no relevant financial relationships.
Ahmed Abdelhakeem indicated no relevant financial relationships.
Mohamed Vadva indicated no relevant financial relationships.
Robert Morrison indicated no relevant financial relationships.
Amr Hamed, MD1, Nigil Thaimuriyil, DO2, Ahmed Abdelhakeem, MD1, Mohamed Vadva, MD3, Robert Morrison, MD4. P2899 - A Pseudoaneurysm Within a Pancreatic Pseudocyst: A Rare Complication Managed With Endovascular Stenting, ACG 2023 Annual Scientific Meeting Abstracts. Vancouver, BC, Canada: American College of Gastroenterology.
